What is it?
Normally, each female ovary at the beginning of the cycle should produce several antral follicles( no more than 10 pieces).Under the influence of hormones, one of them becomes dominant, its capsule is broken and ovulation occurs.
Thus, the ovarian reserve of a woman is spent sparingly and the ability to conceive theoretically is maintained for 45 to 48 years.
When the adrenal cortex is malfunctioned, the production and maturation of antral follicles is destabilized, and in most cases, two pathological conditions arise: multifollicular ovaries( MFN) and polycystic ovaries( PCOS).
Both diseases imply uneconomical expenditure of a woman's ovarian reserve, provoke the development of follicular cysts and make it difficult to conceive. Let's look at multifollicular ovaries, what it is, how they affect pregnancy and how they differ from polycystic ovaries.
Contents of the
- 1 MFIA and PCOS: what's the difference?
- 2 Signs of multifollicular ovaries, results of US
- 3 Pregnancy and multifollicular ovaries
- 4 Treatment of MFIA - hormonal background correction
MFIA and PCOS: what's the difference?
Patients suffering from infertility and forced to often visit ultrasound in different clinics sometimes face the fact that one doctor puts a diagnosis of PCOS on the results of the examination, and another doctor is convinced that the woman has exactly the MPL, and not the polycystosis.
There is also a category of specialists who are convinced that both these diagnoses are identical and should not be shared. Such inferences and differing diagnoses can completely disorient the patient and provoke a gynecologist to prescribe the wrong treatment according to the results of ultrasound.
To avoid such situations, it is better to choose such an ultrasound diagnosisist who is a part-time gynecologist, or one whose practical activity includes only studies of the organs of the female reproductive system.
As a rule, these specialists make ultrasound of ovaries professionally and with much greater competence than general doctors. The difference between these two diagnoses is as follows:
- Echogenicity - determines the tissue density of the organ being examined. With MFN, the echogenicity of the ovaries does not exceed the echogenicity of the uterus. In PCOS, it is much higher, the ovary tissue is much denser than the tissues of the uterus.
- The size of the ovaries - with OIE, the ovaries are slightly larger than normal. Often the values are at the levels of 34 - 37 mm in length and 18 - 22 in width. In PCOS, the length of the ovary is always more than 40 mm, the experienced ultrasound in this case even before the measurements will determine that they are greatly enlarged.
- DEGA hormones and 17-OH progesterone are male hormones produced by the adrenal cortex. With MPL, their values are kept within the normal range( permissible even if they are at the upper limit of the norm).With PCOS, the level of these hormones is always elevated.
- Size of follicles - both diagnoses suggest multiple follicles in the ovaries, but with MFJ, their diameter does not exceed 9 mm. In PCOS, many of these follicles reach a large size, but none can vow.
- Thickness of the follicle capsule - with PCOS the capsule of the follicle is always heavily thickened. Therefore, even if the egg is ripening in it, it can not go outside even if a sufficient amount of the LH hormone is produced in the woman's body. Thus, the follicular cyst is formed. With MFJ, such cysts also occur, but much less frequently( no more than 2 times a year).
- Location of follicles - on the ultrasound machine clearly visible where the follicular apparatus is located. In AMF, the antral follicles are diffusely located. With PCOS, they are almost always located around the periphery, in the shape of a necklace.
It is important that the doctor can diagnose the diagnosis correctly, because the treatment regimens for the multifollicular structure of the ovaries and polycystosis are different, requiring different approaches and techniques.
Symptoms of multifolllicular ovaries, results of ultrasound
Symptoms of MFN can be either indirect or direct, detected by ultrasound. In order to diagnose, the gynecologist is guided by the patient's complaints and ultrasound results.
Manifestations of multifollular ovary syndrome:
- Anovulatory cycles - can be present up to 5 times a year. The causes are either the non-emergence of the dominant follicle, or the appearance of a follicular cyst. The absence of ovulation should be confirmed by the result of folliculometry, rather than being a withdrawal of a woman based on the maintenance of the BT schedule and the use of ovulation tests.
- Infertility - is a consequence of frequent anovulatory cycles. However, in the case of the MFW, it is enough for the spouses, with the help of ultrasound, to catch the moment when ovulation will occur and attempt to conceive. Whereas with PCOS this tactic would not have helped - polycystosis causes a constant absence of ovulation.
- Irregular menstruation - is a consequence of malfunctioning of the ovaries, as a result of which the first phase of the cycle becomes long, and instead of the prescribed 12-14 days it stretches for 30-40 days. Then the second phase begins, which, with multifollicular ovaries, lasts, on average, 8 to 10 days. Thus, it appears that the menstrual cycle of a woman with MPJ is often stretched for 40 to 50 days.
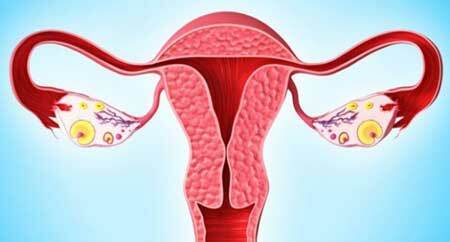
Symptoms of MFIA for ultrasound:
- Ovary slightly enlarged and slightly above the norm.
- Echogenicity of the ovaries is less than the echogenicity of the uterus.
- Multiple antral follicles( more than 20), a size not exceeding 9 mm in diameter.
- The capsule of the dominant follicle is not thickened.
- Antral follicles have a diffuse location in the stroma.
A competent specialist will detect the signs of multifollicular ovaries even at the first visit of ultrasound, even if before a few cycles, folliculometry was not performed to determine the presence of ovulation.
Pregnancy and multi-follicular ovaries

If the conception of the child has already taken place, then the FFM does not affect the bearing in any way. This diagnosis does not provoke an increased production of DHEA and 17-OH progesterone hormones, which would be a threat to the fetus and would require a constant correction at the beginning of pregnancy.
The main difficulty of getting pregnant with multifollicular ovaries lies in the fact that couples find it difficult to achieve regular ovulation in order to be able to try to conceive a child in each cycle.
- There is only one way for this: to eliminate the hormonal failure, which caused the absence of growth of the dominant follicle and endometrium.
If hormone correction does not help - the couple should contact a reproductive gynecologist who will prescribe stimulation of ovulation. Since the beginning of the cycle, a woman will periodically inject drugs that stimulate the growth of the follicle.
Once every 2 days, ultrasound monitoring will be performed, with the help of which the doctor will observe how the ovaries of the patient react to the administration of the drugs.
When the diameter of the dominant follicle reaches its peak, a woman will be injected with hCG, so that the integrity of his capsule is broken, and the egg has the opportunity to go outside and fall into the fallopian tube.
However, when stimulating ovulation you need to take into account:
- first, the dominant follicles can mature a few and all of them within a day are able to vomit.
- secondly, the dominant follicles can mature not in one but in two ovaries, and the ovaries can begin to ovulate together. Therefore, before starting the procedure, the doctor must warn the patient about the high risk of multiple pregnancies.
Treatment of MFIA - correction of hormonal background
Curing multifolllicular ovaries is completely impossible. However, with the help of hormonal correction, it can be achieved that, despite the production of a large number of antral follicles, the ovaries in each cycle will be stably capable of ovulation.
This, firstly, normalizes the cycle, and secondly - it will give the woman a normal opportunity to become pregnant.
Gynecologist-endocrinologist should be engaged in the treatment of hormonal background, the task of which will include the impact on each hormone involved in the process of egg maturation and pregnancy retention. Women with MFJ usually have similar problems with hormones:
- Reduced estradiol - is corrected by preparations containing a synthetic analogue of estrogens, or by herbs-phytoestrogens. This hormone is able to respond quickly to treatment and the results of therapy can become noticeable already in the cycle in which it was started. With MFN, even with the protracted first phase, during the administration of drugs that increase estradiol, a dominant follicle may begin to grow and the endometrial layer thicken.
- Reduced progesterone - also able to respond quickly to therapy. Increases with the help of synthetic analogues of the hormone, which are prescribed in the second phase of the cycle.
- High testosterone - responds slowly to treatment, so it will take several months to bring this hormone back to normal. Natural means to reduce it is almost impossible, so doctors are forced to prescribe to women potent drugs, the dosage of which must be selected very carefully.
If doctors manage to stabilize the hormonal background, then in the presence of multifollicular ovaries it is possible to become pregnant and safely endure the child.
After giving birth, a woman can again begin to pursue anovulatory cycles - but if she is going to plan another pregnancy, hormones can be baptized for a while and produced.