This can continue until the occurrence of certain triggering factors, for example, reduction of protective functions, artificial termination pregnancy, the use of intravaginal contraceptive failure, and even just on the background of widespread common diseases or regular menses.

What it is?
Ureaplasma (Ureaplasma urealyticum) - this is a special type of microbe, occupying their properties and dimensions intermediate between protozoa and viruses. These bacteria easily penetrate into genitourinary system cells and multiply there. Thanks to this unique ability, they easily escape the human immune system.
Ureaplasma referred to as opportunistic vaginal flora - in smears in approximately 60% of clinically healthy women found this kind of microbe. If ureaplasma in women does not give symptoms, and treatment is not required - it is not a disease but a normal variant.
Causes of ureaplasmosis
Directly cause disease becomes entry into the body by any route conventionally pathogen - Ureaplasma which after infection very quickly penetrates the surface epithelium or white blood cells, and can persist in cells for extended indefinitely time.
Manifestirovanie infections can provoke:
- hormonal changes - menstruation, childbirth, abortion;
- Any condition that can lead to a reduction in the overall immunity tension;
- frequent change of sexual partners - in this case several times increases the likelihood of penetration into the body is definitely pathogenic microorganisms that can induce ureaplasmosis;
- Manipulation of urinary or genital organs - establishing or removing the intrauterine device, surgical treatment of women's pathology the reproductive system (moxibustion erosion, removal of cysts and warts) or manipulation mochevyvedeniya organs (catheterization, cystoscopy, cystography).
For a long time the disease can be asymptomatic - disease manifestations occur only in the later stages, when the body is already in any irreversible changes. In this case, women may form adhesions in the pelvis, which can cause infertility or provoke the development of an ectopic pregnancy.
Classification
In fact there are several types of medicine of the infection, but at the present time the main types secrete ureaplasmas women:
- parvum (ureaplasma parvum);
- urealitikum (ureaplasma urealyticum).
These two types may be combined into a single species under the name ureaplasma spetsies. Identify some form of infection is necessary, since in most cases they are interfaced with other diseases.
If Ureaplasma parvum was detected in women, it does not require special treatment activities as normal in women, these microorganisms are present in the normal flora of the genitourinary sphere. Medical assistance may be required only if the number of bacteria exceeds by several times, as this is a threat to an inflammatory process.
symptoms
Symptomatology ureaplasma (see. photo) in the female body are sometimes discovered by chance, by diagnosing other diseases. Under other circumstances, the signs ureaplasmosis recognized without problems.
Here are the main ones:
- Painful sensations. Usually localized in the lower abdomen, occur on the cutting type. In this case, ureaplasmosis very likely given the complications in the uterus and appendages.
- Vaginal discharge. Usually quite scarce, with no smell and color. Along with this, if the inflammatory process is already running, discharge may take a sharp odor and change the color to green, or yellow.
- Problems with sexual function. The patient becomes painful and uncomfortable sex. Discomfort appear during intercourse and stored after the completion thereof.
- Problems with urination. The urge to empty the bladder become more frequent, accompanied by, at the same time, painful feelings, sharp pains, burning.
- Lzheangina. If the infection occurred during oral sex, there may be signs that are typical for anginas: plaque on tonsils (tonsils), painful sensations in the oropharynx, difficulty swallowing, and so forth.
If ureaplasma not cause discomfort, painful feelings, it will still need to be sure to be eradicated. Timely access to a profile expert not allow infection ailment to develop, help avoid complications, including chronic ureaplasmosis (requires a long and complex therapy). It is necessary to monitor their health permanently.
Diagnostics
Such disease as ureaplasmosis, the following methods can be diagnosed:
- Serological method (detection antibody). This method of diagnosis is assigned to identify the causes of abortion, infertility, and diseases of inflammatory nature in the postpartum period.
- Molecular biological techniques. With this diagnosis, you can determine the presence or absence in a test sample ureaplasma. But the number of microorganisms present diagnostic method can not identify.
- Bacteriological (culture method). This diagnosis is based on the cultivation of ureaplasma in an artificial medium. For the study should be taken with a swab of vaginal vault, urethral mucosa. Only the method presented study will determine the amount of Ureaplasma, which is sufficient for the development of this disease. Bacteriological method is considered to be decisive in deciding ureaplasmosis therapy.
Ureaplasma in pregnancy
When planning a pregnancy, the first thing to make a woman, it is to be examined for the presence of ureaplasma. This is due to two reasons. Firstly, the presence of even a minimum amount of ureaplasma in the urogenital system of healthy women during gestation of the child, leading to their activation, resulting in growing ureaplasmosis.
Second, in the early stages of pregnancy can not be held ureaplasmosis treatment (by the way, during this period he the most dangerous to the fetus) because antibiotics negatively affect the growth and proper development fetus. Therefore, it is in advance of pregnancy to identify ureaplasmas, if any, and to heal. The disease is dangerous to the fetus by the fact that during childbirth infection is transmitted to the baby through the birth canal. If a pregnant woman infected ureaplazmozom should be compulsory to consult a doctor for further diagnosis.
To prevent infection of the baby during childbirth, postpartum infection of the mother's blood, as well as to reduce the risk of premature delivery or miscarriage in early pregnancy, pregnant with the disease after twenty-two weeks of pregnancy is carried out antibacterial therapy. Preparations selects the attending physician. In addition to antibiotics, prescribe drugs to boost the body's defenses in order to reduce the risk of secondary infection development.
Effects
By virtue of this fact, and that the disease often occurs in the chronic form, ureaplasmosis expressed invisible symptoms. Women are more likely to seek help only when it emerged the following complications:
- oophoritis - oophoritis.
- Violation of the regularity of the menstrual cycle.
- adnexitis - inflammation, exciting uterine appendages (ovaries, fallopian tubes, ligaments).
- ascending pyelonephritis pathogens detected when the ascent above the bladder to the kidneys.
- Cystitis (Inflammation of the bladder), and chronic urethritis (chronic inflammation of the urethra) arise as a result of ascending infection.
- vaginosis - complication inconvenience and pain during intercourse.
- Secondary infertility, which is a consequence of prolonged inflammation in the cervix and fallopian tubes. Even after adequate treatment ureaplasmosis doctor may discover that the fallopian tubes are impassable for eggs.
In addition to the above, Ureaplasma bacteria can damage the skin and the structure of the egg, making it impossible to conceive a healthy child.

How to treat a woman ureaplasmosis?
Effective treatment ureaplasmosis - it is a long process that requires patience and perseverance of women, as a single short course of medical therapy to eliminate ureaplasmas impossible. In addition, it is very important to a woman stuck to the doctor's recommendations regarding diet and lifestyle.
Patients with ureaplasmosis gynecologists usually prescribed treatment systems, comprising:
- Vaginal.
- Immune-boosting drugs.
- Antibiotic therapy.
- Vitamin therapy.
- Enzymatic agents having antiinflammatory action.
- Restoration of normal microflora by using special drugs (probiotics) inwards and place.
- Physical therapy procedures. Of physiotherapy at ureaplasmosis gynecologists preference is given to magnetic therapy, electrophoresis. Good performance also has an intravenous laser irradiation of blood, mud and pelvic massage.
Antibiotics for ureaplasma
How to cure ureaplasmosis women? Only with antibiotics:
| antibiotics Group | preparations |
| Makrolipidy | Sumamed, Azithromycin. This means the first line, which accumulates in cells at the desired concentration of at least 3 days. |
| tetracycline | Doxycycline, JUnidoks. 10 years ago they were the mainstay of therapy, but now they are administered only in a complex with other antibiotics. And all because of him bacterium adapts quickly. |
| Ftorhinolonidy | Avelox, which can accumulate in the cells for a long time, so taking them durable, more than 21 days. |
Important! When unexpressed inflammation therapy treatment costs only one antimicrobial, and if it is complicated, the treatment regimen will be tandem, e.g., alternation of macrolides and tetracyclines.
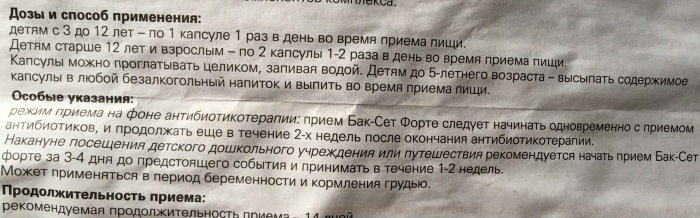
probiotics
That there was candidiasis, along with antibacterial drugs should take probiotics - preparations containing "useful" organisms that make up the normal microflora, or to facilitate their recovery.
The most effective modern probiotics are:
- Laktovit.
- Bifidumbacterin.
- Lactobacterin.
- Linex.
- Narine.
- Biovestin.
In the acute form of the disease systemic antibiotics against the backdrop of probiotics often enough for successful treatment. In subacute form of this treatment it is advisable to complement topical antibiotics (vaginal tablets, douching).
disease prevention
Preventive measures for the prevention of female ureaplasmosis:
- the use of barrier protection means;
- rejection of accidental intimacy with different partners;
- strict adherence to personal hygiene rules;
- constant maintenance of immune system in the proper state (hardening, vitamins, healthy food);
- ureaplasmosis should be treated not only for women, but also among regular sexual partner.
Likely to develop depends on the state of the immune system and the presence of concomitant infections in the body. When hidden currents to determine the disease is impossible, so you need to be inspected by a specialist. When planning a pregnancy should take responsibility for the medical examination of both partners.