Content
- Overview of Tuberculoma
- ICD-10 code
- The emergence of a necrotic formation
- Contagiousness of the disease
- Varieties of tuberculoma
- What is the difference from tuberculosis
- Causes of tuberculoma
- Variants of the course of the disease
- Stable flow
- Progressive tuberculoma
- Regressive course
- Primary and secondary symptoms of pulmonary tuberculoma
- Diagnostic methods
- Recurrent tuberculoma
- Lung lesion treatment options
- The use of chemotherapy
- Surgery
- Traditional medicine as supportive therapy
- Patient prognosis
- Recovery from illness
- Preventive measures
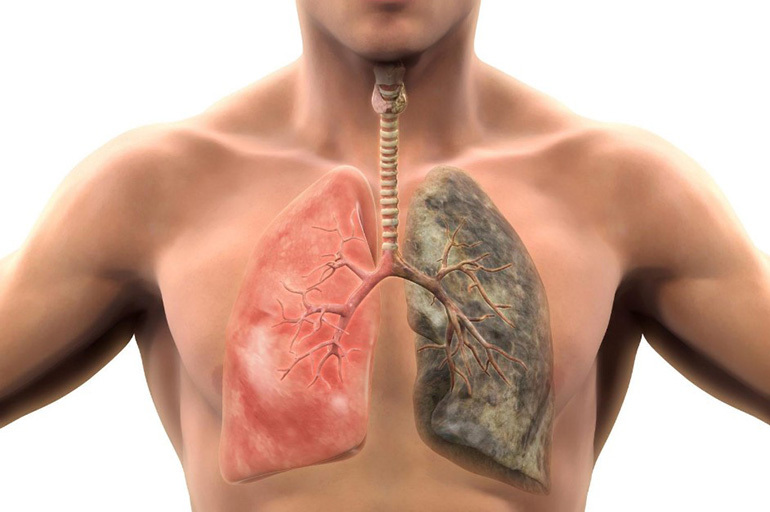
The spread of mycobacterium tuberculosis in the lung tissue leads to the formation of infiltrates, foci of necrosis and decay. A limited capsule with caseous contents (tuberculoma) can be an independent form of the disease or its complication.
For a timely diagnosis, patients from the risk group must understand how pulmonary tuberculoma develops, what it is, the consequences and prognosis of treatment.
Overview of Tuberculoma
Tuberculoma, or tuberculoma, is a volumetric formation, which consists of a zone of cheesy (caseous) necrosis and a dense two-layer capsule. Most often it develops as a result of infiltrative, disseminated or focal pulmonary tuberculosis. In patients with initially diagnosed disease, tuberculomas are found in 4-6% of cases.
The membrane that separates the necrotic focus from the lung tissue consists of granulomas and fibrin fibers. The structure and thickness of the capsule depend on the pathogenesis of secondary tuberculosis.
ICD-10 code
According to the International Classification of Diseases (ICD-10), pulmonary tuberculoma belongs to group A-15. The subgroup of the diagnosis is selected depending on which study confirmed the presence of mycobacteria: histological, bacterioscopic, etc.
In rare cases, caseous-necrotic foci have a different localization. For example, meningeal tuberculoma has the code A17.1.
The emergence of a necrotic formation
The formation of a limited focus of necrosis is the body's response to the vital activity of mycobacteria in the tissues. Under the influence of antibiotics or other factors, inflammation around the tuberculous focus gradually dissolves, and in its place an infiltrate appears, containing curdled-necrotic masses.
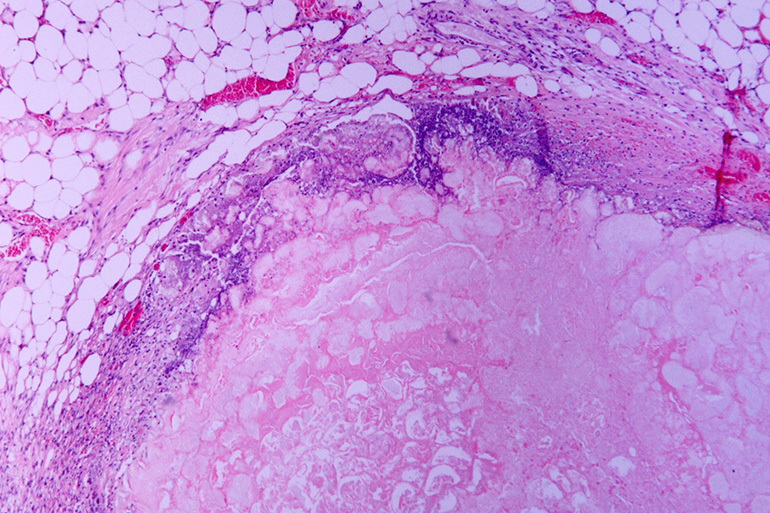
Around the central zone, granulations appear, consisting of young connective tissue and immune cells (lymphocytes, macrophages, etc.). They form the first layer of the capsule, which will further separate the caseoma from healthy lungs. On the periphery, the focus is covered with collagen fibers, which turn into dense fibrous tissue.
The capsule diameter is 12 to 110 mm. The development of pathological education takes 1-3 years.
Contagiousness of the disease
The dense connective tissue membrane prevents the spread of mycobacteria through the lungs and their excretion along with sputum. Thus, isolated tuberculoma is not contagious to others.
However, if the caseous masses have melted the protective shell, then the infection quickly spreads through the bronchogenic route. With the disintegration of the focus, tuberculosis relapses and the area of lung damage increases.
Drained tuberculoma is also dangerous for other people. Communicating with the bronchus, it secretes necrotic masses into the upper respiratory tract.
Varieties of tuberculoma
By morphology, tuberculomas are classified into the following types:
- Infiltrative pneumonic. It develops as a result of incomplete resorption of infiltrates in a secondary disease. In the structure of the focus, caseous zones alternate with epithelioid granulomas. The walls of the connective tissue capsule have a minimum thickness.
- Solitary. The structure of the formation can be homogeneous (uniform) or layered. Homogeneous tuberculoma has a pronounced central zone with a curd mass and a two-layer capsule. Layered foci occur with a wave-like course of the disease. Caseous zones in them are located concentrically and are separated by walls of connective fibers.
- Conglomerate. It is a complex of several caseous foci, which are limited to one common capsule. The structure of the focus is homogeneous. Due to the combination of several zones of necrosis, the capsule is irregular in shape.
Important information: The clinical picture of the course of fibrocavernous pulmonary tuberculosis

According to the size of the formation, they are divided into small (up to 20 mm), medium (from 20 to 40 mm), large (from 40 to 60 mm) and giant (more than 60 mm).
What is the difference from tuberculosis
Difference between types of tuberculosis
| Criterion | Tuberculoma | Primary tuberculosis complex | Focal disease | Infiltrative tuberculosis |
| The nature of development | In most cases, secondary | Primary | Secondary | |
| Localization of foci | In the peripheral segments of the lungs | In segments I and II | Mainly in the upper segments | |
| Contagiousness | Isolation of bacteria is possible only if the membrane is damaged or in contact with the bronchus. | Not contagious | Infectious in decay | |
| Clinical picture | May be asymptomatic | Proceeds with fever and intoxication | Has a blurred picture, pronounced symptoms are observed in only 30% of patients | Features of the course depend on the type of infiltrates |
| X-ray signs | Presence of homogeneous rounded shading | Enlargement of the breast lymph nodes, inflammation of the lymphatic vessels, areas of damage to the lung tissue | The presence of small (up to 10 mm) foci with rounded or blurred contours | The presence of darkening of the corresponding form, with decay - with zones of enlightenment in the center |
| Changes in blood count | With progressive tuberculoma - leukocytosis, increased ESR and other signs | Leukocytosis, neutrophilia, lymphocytopenia, increased ESR | Increased ESR | A shift of the leukocyte count to the left, with small infiltrates, the changes are insignificant |
| Tuberculin test reaction | Negative with isolated capsule | Positive | May be false negative | Positive in most cases, even in the absence of decay and bacterial excretion |
Causes of tuberculoma
Most often, pulmonary tuberculomas develop after secondary forms of the disease: focal, infiltrative, disseminated, etc. In some cases, they are a complication of the disease of the intrathoracic lymph nodes or primary tuberculosis complex.
80% of patients with encapsulated education have previously received antibiotic therapy. The cause of a caseous focus may be an ineffective combination of drugs, improper medication or a long break in treatment.

Hypersensitization of immunity plays an important role in the pathogenesis of the disease. Patients with metabolic disorders (eg, diabetes mellitus) are at increased risk of developing tuberculoma.
Most often, this form of the disease develops in men 20-40 years old.
Variants of the course of the disease
Tuberculoma can be stable, progress or regress. The course of the disease influences the choice of the treatment method and the prognosis of the patient's recovery.
Stable flow
With a stable course of the disease, the formation does not change in size on the roentgenogram, but it can provoke chronic intoxication of the body. The disease proceeds without symptoms or with an erased clinical picture. A wet cough may occur.

Progressive tuberculoma
Progressive tuberculoma is the most aggressive form of the disease, characterized by the presence of inflammation around the capsules. The progression of pathology can be accompanied by such phenomena as:
- loosening of the focus;
- melting of the fibrous membrane;
- the release of caseous masses through the draining bronchus with the formation of a cavity in the place of the capsule;
- infection of the lymph nodes and surrounding lung tissue.
Regressive course
With a regressing course, the caseous contents of the capsule are calcified, and the fibrous membrane is hyalinized. Destruction of connective tissue and its impregnation with plasma proteins leads to scarring of the lesion.
X-ray images may show a decrease in tuberculoma.
Primary and secondary symptoms of pulmonary tuberculoma
In most cases, the formation of an encapsulated focus is asymptomatic. The first signs of pathology may be:
- weakness, fatigue;
- night sweats;
- subfebrile temperature;
- frequent cough (dry or with little phlegm);
- loss of weight and appetite;
- chest pain in the area of foci (with subpleural localization).
Important information: The clinical picture of the development of tuberculous pleurisy in humans

With progressive and drained tuberculoma, a wet cough with an admixture of blood may be observed. The melting of the capsule and the spread of infection leads to an increase in temperature and increased intoxication.
Diagnostic methods
Early diagnosis of the disease is difficult due to several factors:
- erased clinical picture;
- a large number of false negative results of tuberculin tests;
- absence of mycobacteria in bronchial lavages and sputum until the phase of complete disintegration of the capsule.
The most accurate primary methods for diagnosing tubercles are fluorography and radiography of the lungs. On negative images, necrotic lesions appear as rounded formations with smooth or scalloped contours.

With a long course of the disease and large sizes, the tuberculoma capsule may have an irregular or oval shape. In this case, denser calcified inclusions are observed on the periphery. With a conglomerate type of tuberculoma, several foci of different densities are found inside the fibrous membrane.
In some patients, the capsule is connected to the root of the lung with cords or bronchus.
A similar structure on the roentgenogram has a false tuberculoma - a cavity filled with caseous masses. With obstruction of the bronchus, the outflow of the contents of the cavity is difficult, and it forms a dense homogeneous formation.
To exclude a non-infectious etiology of the disease, the patient may be referred for CT, bronchoscopy, biopsy and thoracoscopy. Differential diagnosis of pathology is carried out with a parasitic cyst, aspergilloma, secondary malignant tumors, hamartoma and lung cancer.
In addition to instrumental studies, phthisiatricians also use laboratory methods:
- general blood and urine tests;
- bacteriological examination of sputum and bronchial lavage;
- tests for sensitized lymphocytes (quantiferon test, T.SPOT.TB).

When examining a patient, the doctor performs auscultation of the lungs. Wheezing and pleural rubbing may be signs of tuberculoma. To identify tubinfection, a Mantoux or Diaskintest test is performed, however, due to the isolation of the process, they can give a false negative result.
Recurrent tuberculoma
This form of the disease practically does not recur, but it can turn into caseous, disseminated or infiltrative tuberculosis. Re-development of pathology can occur upon contact with a patient with an active type of disease.
Lung lesion treatment options
Depending on the type, size and complications of tuberculoma, chemotherapy or surgery is prescribed. With small limited foci and a closed form of the disease, it is possible to cure the patient without surgery.
The use of chemotherapy
Chemotherapy includes 4 antibacterial drugs:
- Rifampicin;
- Ethambutol;
- Isoniazid;
- Pyrazinamide.

Within 2-3 months of treatment, a 4-component regimen is practiced, and over the next 4-6 months - a 3-component regimen. With multiple drug resistance or negative dynamics, 5- and 6-component drug regimens are used.
Before curing tuberculosis, the sensitivity of the isolated strain of mycobacteria to antibiotics is determined.
The following methods are used to stimulate immunity and resolve the necrosis focus:
- tuberculin therapy;
- the introduction of hyaluronidase;
- ultrasound and magnetic therapy.
Surgery
Surgical intervention is shown:
- with a large size of the necrotic focus (more than 20 mm);
- the presence of several isolated capsules, conglomerate type of formation;
- acute tuberculous intoxication;
- rapid progression of the disease;
- involvement of the bronchi;
- disintegration of the capsule, which is accompanied by the release of bacteria;
- no response to drug therapy for 3-4 months.

Depending on the size of the focus and the course of the disease, one of 2 types of surgery is performed: removal of tuberculoma or limited resection of the lung. If the infection spreads, a segmentectomy or lobectomy is performed.
Important information: Clinical picture and nuances of the development of infiltrative pulmonary tuberculosis
After the operation, the patient is prescribed anti-tuberculosis antibiotics for a period of 6 months. This reduces the likelihood of relapse and prevents the multiplication of mycobacteria in other sensitized areas of the lungs.
Traditional medicine as supportive therapy
Folk remedies are not a substitute for adequate chemotherapy and surgery, but they can facilitate sputum removal, reduce intoxication, and calm the patient. The most effective are:
- aloe, kalanchoe and echinacea extracts;
- decoction of wheatgrass roots in milk;
- celandine kvass;
- infusion of moss, barley, oats and bear;
- beekeeping products (honey, bee bread, propolis and podmore);
- decoction of oats and bran;
- infusions of mother-and-stepmother, oregano (oregano), clover, wild rose, St. John's wort;
- decoction of raisins and barley.

Some healers also use milk conspiracies.
Patient prognosis
Specific anti-tuberculosis therapy leads to a complete cure of the patient in 95% of cases. 5% of patients develop severe complications: respiratory failure, atelectasis (collapse) of the lung, massive bleeding, etc.
In the absence of treatment, the active form of the disease gradually develops. Due to the dissemination of mycobacteria in the phase of disintegration of the formation, a segment or a whole lobe of the lungs is affected.
Premature termination of therapy, unauthorized dose reduction and missed medications can lead to the emergence of drug-resistant strains of Koch's bacillus. Treatment of patients with resistant forms of tuberculosis requires the use of regimens of 5 or more antibiotics at maximum dosages.
Recovery from illness
Recovery from illness takes 1 to 2 years. Patients should receive a nutritious diet rich in proteins, fats and vitamins.

After completion of chemotherapy, patients are shown spa treatment. Mineral baths, aerotherapy, sea bathing, etc. contribute to recovery.
Preventive measures
To prevent the development of tuberculoma, the same methods are used as for the prevention of other forms of the disease. To minimize the risk of developing pathology, you need:
- stop drinking alcohol, smoking and taking drugs;
- eat well, include fruits and vegetables in the diet;
- devote 8-9 hours a day to sleep at night;
- timely treat foci of chronic inflammation in the body;
- follow a diet and undergo specialized examinations for metabolic diseases (diabetes mellitus, thyroid diseases, etc.);
- take vitamin and mineral complexes during epidemics, increased physical exertion, stress and therapy of infectious diseases;
- use personal protective equipment when in contact with patients with tuberculosis, as well as working with toxic substances, metal, construction and wood dust;
- annually undergo a preventive medical examination and fluorography.
A measure of the prevention of tuberculoma during treatment is the exact observance of the recommendations of the phthisiatrician.
For people at risk, revaccination of BCG is indicated in adulthood. This group includes:
- residents of regions with a poor epidemiological situation;
- staff of TB dispensaries, infectious diseases hospitals, diagnostic laboratories;
- family members of patients with tuberculosis;
- patients with various forms of immunodeficiency (vaccinated with an inactivated vaccine).
Upon contact with a patient with an open form of the disease, a preventive course of antibiotics is prescribed, which lasts for 3-6 months. A prophylactic course may include taking Isoniazid, Rifampicin, Protionamide, Cycloserine, Pyrazinamide, Kanamycin, Viomycin and other drugs.