Content
- Briefly about the pathogen
- ICD-10 code
- Pathogenesis (occurrence and development) of the disease
- Causes of primary tuberculosis
- Transmission routes
- For children and adolescents
- For adults
- Risk group
- Primary symptoms
- Chronically current primary tuberculosis
- Differences from secondary tuberculosis
- Forms of the course of the disease
- Tuberculous intoxication
- The defeat of the intrathoracic lymph nodes
- Primary tuberculosis complex
- General diagnostic methods
- Possible complications
- In adult patients
- In children
- Treatment of primary tuberculosis
- Recovery period
- Disease prevention
- Features of tuberculous intoxication in children
- What happens in the child's body
- Symptoms of the disease
- Diagnostic measures
- Treatment of tuberculous intoxication in children
- Forecast and consequences
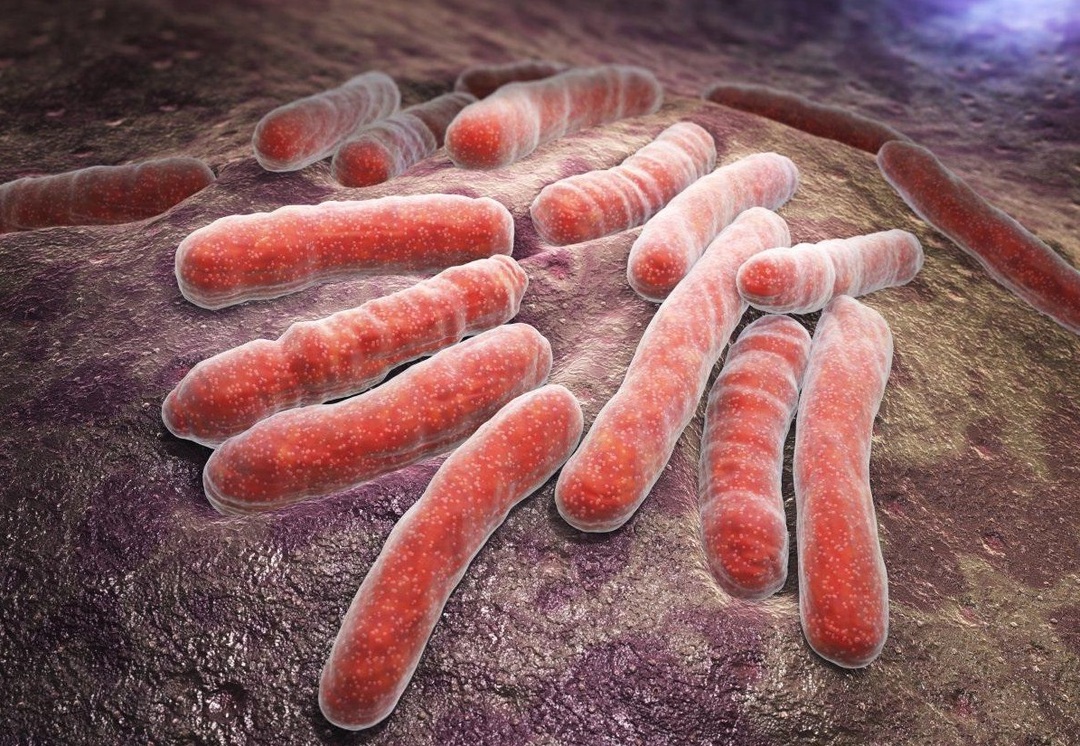
Primary tuberculosis is an infectious pathology that occurs during the first contact of a person with mycobacteria. More common in children. This is a collective concept that includes intoxication, primary tuberculosis complex and damage to the intrathoracic lymph nodes.
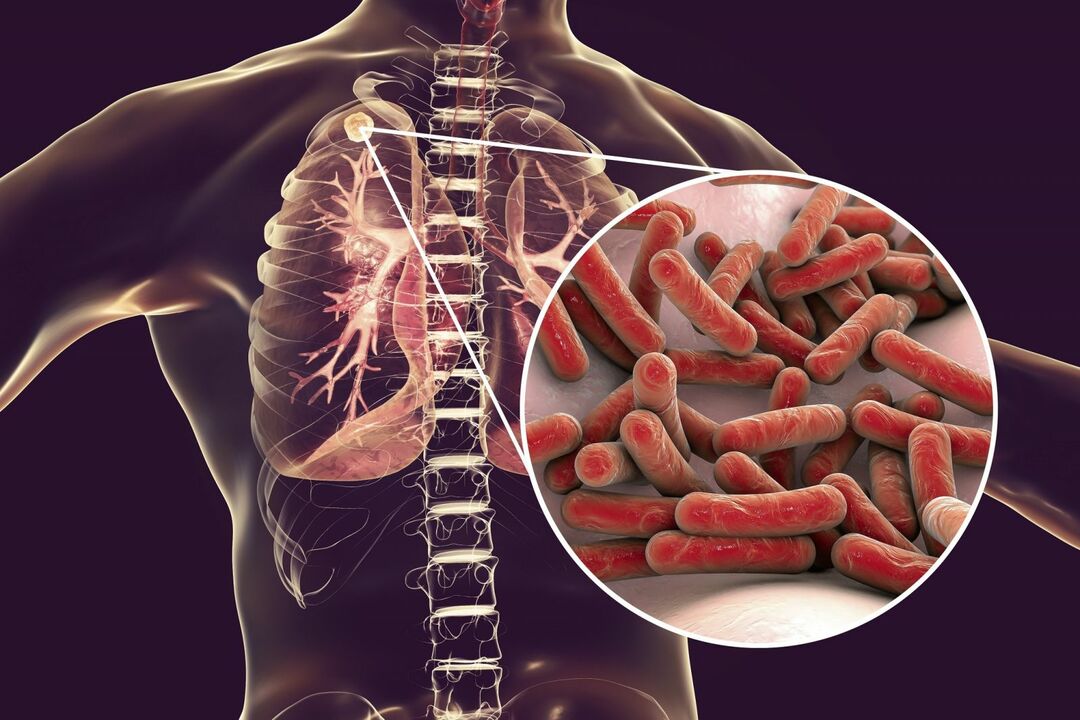
Briefly about the pathogen
Mycobacteria are microorganisms that have the following distinctive features:
- belong to gram-positive bacteria;
- capable of parasitizing inside cells;
- have a size up to 10 microns;
- rod-shaped;
- resistant to acids and many antibiotics;
- are able to change their antigenic structure and morphological properties;
- do not form capsules and spores;
- can exist in L-forms;
- motionless;
- grow on simple nutrient media;
- resistant in the external environment (withstand heating up to 60ºC, up to 10 months stored in the dried sputum of a sick person);
- sensitive to sunlight.
They are transmitted from a sick person to a healthy person through the air and objects.
ICD-10 code
The ICD-10 code for this disease is A15-A19. The concept of primary tuberculosis includes all cases of the disease (confirmed and not confirmed by laboratory), with the exception of secondary forms (focal, infiltrative, disseminated, miliary, cavernous, cirrhotic, fibro-cavernous, caseous pneumonia and tuberculomas).
Pathogenesis (occurrence and development) of the disease
Tuberculous infection and specific inflammation develop as a result of infection with mycobacteria. The causative agent of the disease is found in the macropreparation of patients. The pathogenesis of the primary complex is based on:
- contact with the pathogen;
- granulomatous inflammation;
- the emergence of a primary affect (affected area);
- lymphadenitis and lymphangitis;
- sclerotic changes;
- caseous necrosis (in severe cases);
- calcification (salt deposition and tissue hardening).
A feature of tuberculosis of the intrathoracic lymph nodes is that the lymphatic vessels are not inflamed, there is no infiltration in the lungs. The pathogenesis is based on hyperplasia of lymphoid tissue (its increase in volume), specific inflammation and the formation of a zone of necrosis (caseosis).
The process involves paratracheal, bronchopulmonary or bifurcation nodes. In the chronic course of the disease, the foci become denser or melt.
In the case of tuberculous intoxication, when mycobacteria enter the lungs, specific inflammation does not develop. The pathogen enters the vessels and spreads throughout the body. Bumps (granulomas) form in the tissues. This is a specific reaction to the penetration of bacteria. Weakened people (with diabetes, cancer, alcoholism) develop a pronounced intoxication of the body.
Causes of primary tuberculosis
The disease begins after infection with pathogenic strains of mycobacteria. This is possible directly from a sick person or indirectly (through household items).
Primary pulmonary tuberculosis often develops in children at the first contact with bacteria. Adults are less likely to get sick.
Predisposing factors include:
- physical stress;
- stress;
- poor nutrition (lack of vegetables, berries, fruits in the diet);
- acute lack of vitamins;
- living in the same apartment with the patient;
- smoking;
- addiction to alcoholic beverages;
- primary immunodeficiency;
- stay in dark, unventilated and humid rooms.
Transmission routes
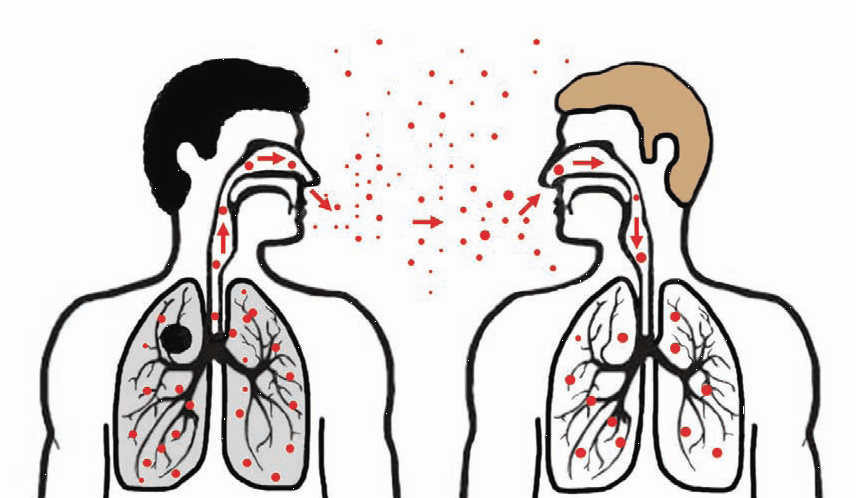
Phthisiology identifies the following methods of transmission of mycobacteria:
- Airborne. It occurs in 90% of cases. A patient with active tuberculosis dispels bacteria when coughing and sneezing along with sputum. The pathogen can spread to 8-9 m and enter the respiratory tract of other people.
- Air-dust. Mycobacteria settle on dust and rush upward with a stream of air. So they get into the nose and mouth, and from there - into the trachea, bronchi and lungs.
- Contact and household. It is realized through various household and personal hygiene items (towels, toothbrushes, dishes).
- Food grade. Infection occurs when eating the meat of a sick animal (cattle), milk, or through dirty hands.
- Vertical (to a child from a future mother in utero).
Important information: Features of the development and course of miliary pulmonary tuberculosis
The main mechanism of infection is aerogenic.
For children and adolescents
Mycobacteria enter the child's body by air, food, contact-household and mixed routes. Possible infection during childbirth and by swallowing amniotic fluid.
Most often, infection occurs at home from adults. Less often - in kindergartens, schools and other organized groups. There are cases of nosocomial infection. Children under 2 years of age are most susceptible to tuberculosis.
For adults
Adults in most cases become infected through the air. It is possible to get an infection when using the same dishes with a patient, during kissing, when visiting an anti-tuberculosis dispensary, where sick relatives are lying, in public places.
It is highly likely to become infected by contact with coughing people with an active form of the disease.
Risk group
It includes the following categories of people:
- HIV-infected;
- children born to sick mothers;
- unvaccinated;
- smokers;
- persons suffering from alcohol dependence;
- patients with diabetes mellitus and leukemia;
- having chronic diseases.
People with weakened immune systems have a low resistance to infection. This is possible after a course of chemotherapy or radiation, with insufficient physical activity, drug addiction, endocrine pathology and taking immunosuppressants (corticosteroids, cytostatics).
Primary symptoms
Manifestations depend on the clinical form of tuberculosis. The most common signs of the disease:
- increased body temperature;
- dry or productive (phlegm) cough;
- sweating;
- weakness;
- malaise;
- dyspnea;
- chest pain;
- swollen lymph nodes;
- weight loss;
- loss of appetite;
- pallor of the skin.
The early period of primary tuberculosis infection can be poor or asymptomatic.

Chronically current primary tuberculosis
It is characterized by a long course with phases of exacerbation and remission. Chronically current primary tuberculosis can last for several years. Often it proceeds under the guise of another pathology (chronic bronchitis).
Differences from secondary tuberculosis
Primary and secondary tuberculosis have different pathogenesis and clinical presentation. Secondary forms occur with hematogenous or lymphogenous spread of mycobacteria. Against the background of repeated contact with the pathogen, a pronounced inflammatory reaction with tissue infiltration develops. In secondary forms of tuberculosis, local lung damage is combined with general symptoms of intoxication. Also, with this pathology, other organs are often affected (skin, kidneys, bones, membranes of the brain), paraspecific reactions occur.
Forms of the course of the disease
Allocate:
- tuberculosis of the intrathoracic lymph nodes;
- primary complex;
- tuberculous intoxication.
Distinguish between pulmonary and extrapulmonary infections.
Tuberculous intoxication
This pathology is characterized by intoxication of the body and the absence of local foci in the lungs and other organs. It accounts for about 10% of all cases of primary tuberculosis. Mostly children are ill. The disease is acute and chronic. Tuberculous intoxication is indicated by the absence of X-ray changes and a positive Mantoux test (diaskintest).
The defeat of the intrathoracic lymph nodes
With this form of the disease, exclusively the intrathoracic lymph nodes are affected without the involvement of the lymphatic vessels and lung tissue. Infiltrates are not detected. The disease occurs in young people 18-25 years old and children. This pathology is characterized by a long course and slow regression. The most severe tuberculosis occurs in children under 3 years of age. There are the following forms of this pathology:
- tumor-like;
- small;
- infiltrative.
Important information: Information about Koch's pathogenic bacillus
Primary tuberculosis complex
It is often asymptomatic and subacute. Less often, the clinic resembles pneumonia. Children and adolescents are ill. The components of the complex are primary affect, lymphangitis and lymphadenitis.
General diagnostic methods
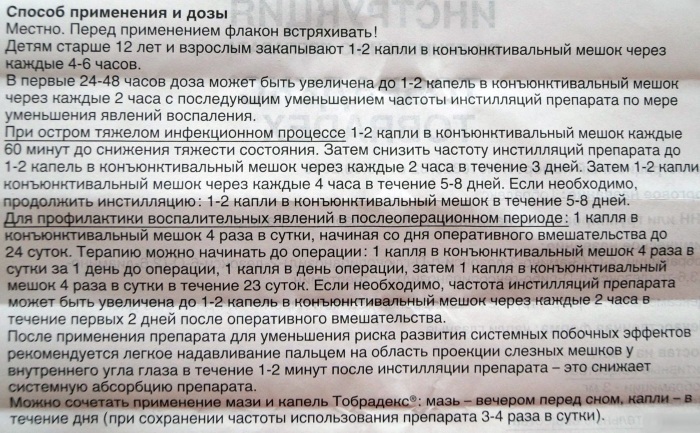
If you suspect tuberculosis, you should contact a phthisiatrician, general practitioner or pediatrician. To make a diagnosis, you need:
- Collecting anamnesis of life and illness. The doctor identifies the main complaints, risk factors, possible conditions of infection, routes of transmission of the pathogen, contact persons and the source of infection.
- Physical examination. Includes auscultation of the lungs and heart, percussion, pressure measurement, palpation of the lymph nodes, counting the respiratory rate and pulse.
- Visual inspection. With the development of bronchoadenitis against the background of tuberculosis of the intrathoracic lymph nodes, the expansion of small vessels in the chest and back is revealed.
- Clinical analyzes of blood and urine. Intoxication is indicated by leukocytosis, accelerated ESR, shift of the formula to the left and eosinophilia.
- Bacteriological analysis of sputum and swabs. Mycobacteria are not detected.
- Tuberculin tests (diaskintest, Mantoux). The reaction is pronounced or hyperergic. A valuable diagnostic criterion is the bend of the samples (the first positive result after all negative ones).
- X-ray examination of the lungs. In the primary tuberculous complex, a slight rounded darkening (primary affect) and signs of lymphadenitis are revealed. With a long course, a Gon focus up to 1 cm in size and calcifications appear. In tuberculosis of VLHL, there is a change in the roots of the lungs.
- Quantiferon test.
- Bronchoscopy.
- T-Spot enzyme immunoassay.
- CT scan.
- Bronchoscopy.
- Lymph node biopsy. The pathology of the disease is being studied. In tuberculosis, mycobacteria and immune cells are found in the dropout foci.
Possible complications
The most often observed (regardless of the localization of the pathological process):
- spread of infection to other organs and systems (damage to the skin, eyes, kidneys, bladder, brain);
- development of secondary pulmonary and extrapulmonary tuberculosis;
- inflammation of the lining of the brain (meningitis);
- the formation of fistulas between the lymph nodes and bronchi;
- bleeding;
- the formation of bronchiectasis (zones of expansion of the alveoli);
- atelectasis (decreased airiness of the lungs);
- broncholithiasis (the appearance of stones in the lumen of the bronchi);
- hemoptysis;
- violation of the heart (with intoxication);
- cachexia (wasting);
- pleurisy;
- hepatosplenomegaly (enlargement of the liver and spleen).
In adult patients
In adults, against the background of tuberculosis, secondary forms often occur (focal, miliary, cavernous). In this case, pulmonary fibrosis, necrosis, the formation of an abscess and tissue decay cavities, sepsis are possible.
In children
The most common complications in children are weight loss, physical retardation, severe asthenic-vegetative syndrome, atelectasis, emphysema and chronic cardiopulmonary failure.
Treatment of primary tuberculosis
All variants of the course of tuberculosis are treated after a medical consultation in a hospital setting. The duration of therapy is from 6 months to 1.5 years.
The criteria for recovery were negative tuberculin tests and bacteriological tests, no clinic, and a normal x-ray picture.
Treatment for the primary form of tuberculosis is aimed at eliminating the symptoms of the disease, preventing progression, cleansing tissues from mycobacteria and preventing complications. Complex therapy involves:
- Oral or injection (intramuscular) use of anti-tuberculosis chemotherapy drugs. 3-4 drugs are prescribed at once. Start with 1 line drug. These include Streptomycin, Pyrazinamide, Ethambutol, Rifampicin, and Isoniazid. They can be replaced with combined agents (Rifacomb, Phthisoetam). In case of intolerance, ineffectiveness or inability to use these drugs, 2 line drugs are used (cephalosporins, Cycloserine, Kanamycin).
- The use of auxiliary agents (hepatoprotectors, immunomodulators).
- Physiotherapy. In case of intoxication, plasmapheresis is effective.
- Diet - to enrich the body with vitamins and nutrients. Vegetables, meat, seafood, nuts, herbs, juices, berries and fruits are useful.
- Respiratory gymnastics.
- Surgical intervention. It is required for the formation of tuberculoma, suppuration, sepsis, empyema, destruction of tissues and cavities.
- Compliance with bed rest.
- Drink plenty of fluids.
- Detoxification measures (with tuberculous intoxication).
Important information: The clinical picture of the course of intestinal tuberculosis in an adult
Recovery period
It is advisable to send children who have recovered to specialized schools and kindergartens. They are put on dispensary registration. Spa treatment is of great importance during the rehabilitation period. To strengthen the immune system, it is recommended to take multivitamins (Supradin, Vitrum Kids, Complivit, Vitrum).
Much attention is paid to the nutrition of children. The following foods must be present in the diet:
- fresh berries and fruits;
- vegetables;
- meat;
- Fish and seafood;
- greens;
- nuts;
- soups;
- porridge;
- cottage cheese and other dairy products;
- eggs;
- juices.
Surgical interventions, travel, flights, stressful situations, physical overload and vaccinations are not recommended immediately after illness. Parents need to help their children overcome physiological problems and provide psychological comfort. Adults in the recovery period need to give up smoking and alcoholic beverages.

Disease prevention
Distinguish between primary, secondary and tertiary prevention of tuberculosis. The classification highlights specific and non-specific preventive measures. The first is immunization. It involves the introduction of the BCG or BCG-M vaccine to children during the first week of life and at 6-7 years of age.
The drug is available in the form of a lyophilisate (powder) to obtain a solution. The composition includes weakened, live mycobacteria. They form a stable immunity to tuberculosis in the vaccinated person. Contraindications are prematurity, intolerance to components, malignant tumors, acute infections and primary immunodeficiency. The solution is injected intradermally.
Non-specific preventive measures are:
- increase in general resistance;
- exclusion of contact with carriers of infection and patients;
- periodic fluorography (once a year);
- periodic medical examinations;
- conducting a Mantoux test in schools and kindergartens;
- isolation of patients and their timely treatment;
- sanitary and educational work;
- taking vitamins;
- wearing personal protective equipment (masks) in contact with patients.
Features of tuberculous intoxication in children
This is a clinically pronounced form of the disease. It often proceeds like influenza and ARVI. The source is most often a patient with an active (open) form, in which mycobacteria, along with sputum, are released into the external environment.
What happens in the child's body
Pathological anatomy distinguishes the following processes occurring in the body of children with tuberculosis:
- specific, granulomatous inflammation;
- bacteremia (entry of the pathogen into the bloodstream);
- the formation of granulomas in the lymph nodes;
- pronounced immune response.
Symptoms of the disease
Early intoxication may be accompanied by headache, loss of appetite, tearfulness of children, general fatigue, deterioration sleep, low-grade fever, sweating, dyspepsia (abdominal pain, stool disorder), swollen lymph nodes and pallor skin. Erythema nodosum and other skin symptoms (congestive infiltrates) are common.
Late intoxication is characterized by lymphopolyadenitis (damage to a large number of lymph nodes), inflammation of the eye structures, hypotension, tachycardia, fever, and weight loss.
Diagnostic measures
The diagnosis is made on the basis of the results of the survey, examination, radiography, tuberculin tests and clinical tests. Samples are positive.
Treatment of tuberculous intoxication in children
Treatment includes chemotherapy (use of 3-4 antibiotics at once), good nutrition, desensitization of the body and rest in a sanatorium. The drugs are taken for a long time and continuously (up to a year).
Forecast and consequences
With timely therapy, doctors predict a favorable outcome of the disease. Drug therapy reduces the risk of developing more severe forms of tuberculosis.