Content
- General concept of intestinal tuberculosis
- Reasons for the appearance
- Infected or not: transmission routes
- Symptoms and Signs
- Initial
- Extraintestinal manifestations
- With the progression of the disease
- Pathological anatomy
- Macroscopic changes
- Histological
- The clinical picture of the course of the disease: forms
- Diagnostic methods
- Treatment principles
- Medication
- Additional therapies
- Nutrition and diet for intestinal tuberculosis
- Recovery prognosis
- Possible consequences and complications
- Preventive actions
Intestinal tuberculosis is a chronic infectious disease caused by mycobacteria. This pathology is relatively rare. Most often, it develops secondarily with the spread of mycobacteria throughout the body. Untimely treatment of tuberculosis leads to intestinal bleeding, difficulty in defecation, peritonitis, acute appendicitis and other complications.
General concept of intestinal tuberculosis
Intestinal tuberculosis refers to the extrapulmonary forms of the disease. It is primary (with foodborne mycobacterium infection) and secondary (against the background of lung damage).
There is an increase in the number of patients with this form of tuberculosis. At the same time, the poor clinical picture often complicates diagnosis and treatment.
Reasons for the appearance
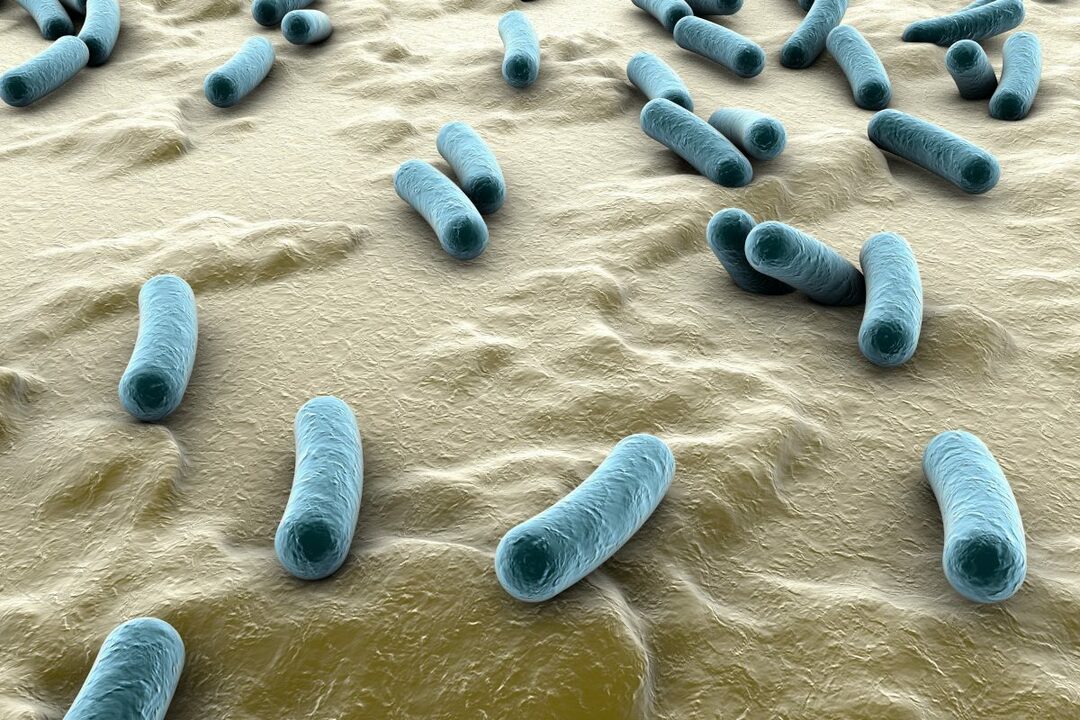
The cause of intestinal damage is the penetration of mycobacteria into the body.
These microorganisms have the following characteristics:
- are intracellular parasites;
- persist in tissues for a long time;
- able to form L-shapes;
- are highly resistant to the external environment;
- have developed resistance to many drugs;
- are rod-shaped;
- resistant to alkalis, acids and drying;
- multiply outside and inside cells;
- cannot move independently;
- have dimensions of 1-10 microns;
- are able to change their morphology and genotype;
- are highly pathogenic;
- produce toxins (cord factor).
The risk of developing the disease is higher in physically weakened persons, the elderly and children.
The contributing factors are:
- the presence of foci of chronic infection (pyelonephritis, hepatitis, chlamydia);
- oncological pathology;
- recent irradiation;
- chemotherapy;
- primary immunodeficiency;
- hypovitaminosis;
- poor nutrition (lack of animal protein, vegetables, berries and fruits);
- smoking;
- alcoholism;
- poor living conditions (high humidity, low temperature);
- frequent acute respiratory infections;
- untimely or irrational treatment of pulmonary tuberculosis;
- contact with sources of infection or living together with them;
- inactive lifestyle;
- taking drugs that suppress immunity (corticosteroids, cytostatics);
- insufficient sleep;
- stress;
- endocrine pathology;
- stay in places of deprivation of liberty.

Infected or not: transmission routes
The following mechanisms of tuberculosis infection are distinguished:
- aerogenic (through the air, when the pathogen spreads with microparticles of sputum when sneezing and coughing);
- contact (through dirty hands and objects);
- vertical (from a sick mother to a child);
- fecal-oral (through the mouth).
The primary form of the disease develops after the first contact with mycobacteria. Infection occurs through food. Transmission factors can be dirty hands, milk from sick animals, contaminated food, dishes, and toothbrushes of a sick person.
A person swallows bacteria. They enter the mouth, esophagus, stomach and intestines. Hydrochloric acid does not act on them, therefore bacteria easily penetrate into the lower gastrointestinal tract, and then into the mucous membrane and cells.
The secondary form occurs against the background of the primary tuberculosis complex, lesions of the intrathoracic lymph nodes and tuberculous intoxication with their untimely treatment. In this case, mycobacteria enter the intestine by hematogenous (through the blood), lymphogenous (through the lymphatic vessels) and deglutational (when swallowing their own sputum with microbes) methods.
Important information: What is primary tuberculosis complex
Symptoms and Signs
With the intestinal form of tuberculosis, there are no specific symptoms. Latent course of the disease is often observed. Most often, dyspepsia (indigestion), malaise, weakness, decreased performance, sweating at night, and a drop in body weight occur. The disease proceeds with periods of exacerbation and remission.
Initial
The first complaints may appear 5-10 years after infection. A long incubation period is characteristic.
The earliest symptoms are:
- Pain in the abdomen. With the defeat of the small intestine, it is localized in the epigastric region, in case of inflammation of the mucous membrane of the ileum - on the right (just below the navel). Most often, the pain is diffuse and of low intensity. The cause of its occurrence is a specific, granulomatous inflammation of the intestinal mucosa. Bumps form in it, which causes pain when food moves.
- Nausea.
- Vomit.
- Alternating loose stools and constipation.

Extraintestinal manifestations
If the intestinal lesion was preceded by pneumonia, then the following symptoms are possible:
- chest pain;
- cough with thick phlegm;
- wheezing;
- malaise;
- increased body temperature;
- sweating;
- weakness;
- swollen lymph nodes;
- hemoptysis;
- pain in the side.
In severe cases, symptoms of chronic respiratory failure (shortness of breath, cyanosis) are possible.
With the progression of the disease
With the development of tuberculosis, pain increases. It becomes permanent and is most often felt in the right iliac region. Low-grade fever, decreased appetite, and weight loss are common. The reasons for the intensification of symptoms are the formation and disintegration of caseous foci. They represent the dead tissue of the intestine.
Pathological anatomy
To recognize tuberculosis, an examination of the mucous membrane is required. Endoscopic examination reveals hyperemia (redness), edema, signs of hypertrophy (thickening and tuberosity), ulcerative defects. The disease is indicated by a “niche” symptom, uneven contours, thickening of folds and their smoothness. The intestinal lumen is reduced. In tuberculosis, healthy areas alternate with affected areas.
Important information: Clinical picture and nuances of the development of infiltrative pulmonary tuberculosis
Macroscopic changes
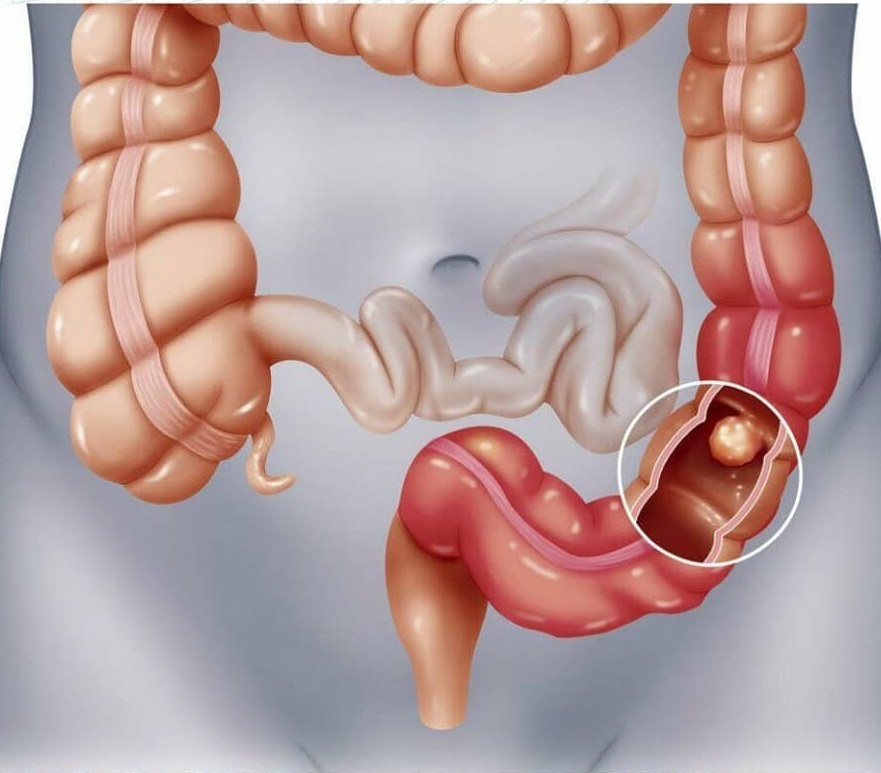
When examining an organ, the following can be determined:
- edema;
- thickening of the mucous membrane;
- pseudopolyps;
- ulcers;
- stiffness of the walls.
The defeat is not total, as in ulcerative colitis.
Histological
A tissue biopsy is required to confirm the diagnosis. The material for the study is fragments of the intestinal mucosa and submucosa. The main histological sign is the presence of a specific granuloma. It contains lymphocytes, epithelioid cells, multinucleated cells and Pirogov-Langhansa cells. In severe cases, zones of caseous necrosis are found.
The clinical picture of the course of the disease: forms
There are the following forms of tuberculosis:
- asymptomatic (inflammation is detected only by instrumental and laboratory methods);
- oligosymptomatic (dyspepsia is observed);
- clinically pronounced.
A complicated type of disease with purulent inflammation of the peritoneum and abdominal organs is distinguished.
Diagnostic methods
The most informative are the following diagnostic methods:
- Patient interview. It is possible to suspect tuberculosis if there are indications of contact with patients, stay in prisons, or previous lung infections in the anamnesis.
- Physical examination (listening to the lungs and heart, palpation of the abdomen).
- Tuberculin tests (Mantoux and Diaskintest). They are not always positive.
- Quantiferon test. The material is blood.
- T-SPOT.TB. Allows to count lymphocytes sensitized to mycobacteria.
- Radiography of the lungs and abdominal organs. It can be carried out with the use of contrast agents.
- FEGDS (fibroesophagogastroduodenoscopy).
- Colonoscopy (examination of the large intestine with a tube with a camera).
- Endoscopic biopsy.
- Histological and cytological analyzes.
- Laparoscopy (examination of organs through a small opening).
- Ultrasound.
- CT scan.
- Clinical analyzes of blood and urine. Lymphocytosis, accelerated ESR, and changes in the ratio of proteins are often detected.
- Fecal occult blood test. Required to exclude oncological pathology.
Differential diagnosis is carried out with duodenal ulcer, Crohn's disease, colorectal cancer, enteritis, ulcerative colitis, diverticulosis, polyps, tumors and proctitis.

Treatment principles
Patients with intestinal tuberculosis are hospitalized. Treatment is predominantly conservative. Its main tasks are the destruction of mycobacteria, relieving the well-being of patients, eliminating symptoms, preventing complications and restoring normal digestion.
Treatment is complex and includes:
- the use of anti-tuberculosis and symptomatic drugs;
- adherence to a strict diet;
- physical rest.
The main principles of therapy are continuity, safety, staging and duration.
Medication
In the intestinal form of tuberculosis, first-line drugs are used - Streptomycin (most effective for primary infection), Pyrazinamide, Ethambutol, Isoniazid and Rifampicin. Several drugs are prescribed at once. An alternative is the use of combined funds. These include Rifacomb, Phtizoetam and Repin B6 (effective for newly diagnosed tuberculosis).
In case of ineffectiveness or inability to use 1st line drugs, 2nd line drugs are prescribed (Moxifloxacin, Kanamycin, Ofloxacin, Cycloserine). Additionally, symptomatic agents are used (antispasmodics, prokinetics, eubiotics). Drug treatment can last up to a year or more.
Additional therapies
Additional methods of treating extrapulmonary tuberculosis include rest in a sanatorium, physiotherapy (ozone therapy), increased immunity and diet. With the development of complications (bleeding, intestinal obstruction, fistulas, peritonitis), surgical intervention may be required.
Important information: The clinical picture of the course of fibrocavernous pulmonary tuberculosis
Nutrition and diet for intestinal tuberculosis
When the body is depleted, table number 11 is shown.
Patients need:
- give up spicy, coarse, fatty, smoked and fried foods;
- enrich the diet with meat, fresh fruits, berries and vegetables;
- eat 4-6 times a day;
- refuse coffee, spices, semi-finished products, carbonated water and alcoholic beverages;
- eat steamed or boiled dishes.

Recovery prognosis
The prognosis is relatively unfavorable. This is due to the late diagnosis of diseases and the development of complications. Timely treatment improves the prognosis. Full recovery is possible.
Possible consequences and complications
The most common complications of intestinal tuberculosis include:
- The defeat of the appendix of the cecum (appendicitis). Characterized by acute pain (first diffuse, and then in the right iliac region), vomiting, fever, stool disorder.
- Fistula formation.
- Peritonitis (inflammation of the peritoneum). Manifested by intestinal obstruction, nausea, high body temperature, stool and gas retention, vomiting, pressure drop, increased palpitations, acrocyanosis, abdominal pain, forced position of the body (on the side with pressed legs), pallor of the skin and confusion consciousness.
- Intestinal bleeding. It is manifested by an admixture of blood in the feces. Possible melena (dark, loose stools with clotted blood).
In some patients, perforation (perforation) of the organ wall occurs.
Preventive actions
A specific preventive measure is timely immunization with BCG or BCG-m vaccine in childhood. To prevent secondary intestinal tuberculosis, it is recommended to timely and correctly treat the underlying disease (primary forms).
Non-specific preventive measures include:
- increased immunity (refusal from cigarettes and alcohol, good nutrition, sports, hardening);
- elimination of stress;
- taking vitamins;
- limiting contact with patients;
- washing hands before eating;
- boiling water and thorough heat treatment of meat.
These measures reduce the likelihood of developing an infection and facilitate the course of the disease.
