Content
- Pathogenesis of the primary tuberculosis complex
- Variability of mycobacterium
- More about the causes
- Infection routes
- Components of the primary tuberculosis complex
- Stages of the disease
- Pneumonic (lung damage)
- Resorption of infiltrate
- Compression
- Calcification (salt deposition)
- Symptoms of the disease
- In children and adolescents
- In the event of an adult
- Types of disease course
- Identification of the primary tuberculosis complex
- Laboratory diagnostics
- X-ray
- Treatment methods
- Surgical intervention
- Chemotherapy use
- Bronchial block (valve installation)
- Recovery period
- Complications and consequences
- Prevention for the risk group
- Primary measures
- Secondary activities
- Useful materials
The primary tuberculosis complex is an infectious and inflammatory disease that develops upon the first contact with mycobacteria. Most often, children and people with reduced immunity are sick. In the absence of proper drug treatment and a complicated course of the disease, secondary forms of tuberculosis develop.

Pathogenesis of the primary tuberculosis complex
This pathology is based on the following processes:
- Ingestion of mycobacteria. Most often, infection occurs by aerogenic (through the air). Contact-household transmission is possible. In some cases, the infection is carried out by food. For an inflammatory reaction to occur, a large number of mycobacteria must enter the body.
- Formation of primary affect. The subpleural regions are most often affected.
- Caseous changes in tissues. Necrosis is observed with the formation of a white curdled mass.
- The defeat of the alveoli and bronchioles.
- Perifocal inflammatory response.
- Damage to regional lymph nodes and blood vessels.
- Formation of the primary focus of Ghosn. A pathological zone of granulomatous inflammation is formed up to 1-1.5 cm in size. In the future, the focus is encapsulated and scarred. In this area, mycobacteria can remain viable, and a repeated inflammatory reaction develops under favorable conditions.
- Calcification (deposition of calcium salts).
Variability of mycobacterium
A distinctive feature of mycobacteria is their ability to change their morphology and antigenic structure.
As a result, resistance to drugs (antibiotics) increases and immunity is suppressed (the body does not recognize microbes well).
Mycobacteria are capable of forming L-forms. They play an important role in maintaining immunity. With a decrease in the reactivity of the body, they are sharply activated and cause inflammation.
More about the causes
The reason for the development of tuberculosis is infection with mycobacteria. These are intracellular microbes that are highly resistant to environmental factors. They are able to persist for a long time on objects and in sputum. This pathology often develops in people in contact with patients with active tuberculosis, and children at the first contact with mycobacteria.
The contributing factors are:
- Decreased immune status (with HIV infection, chlamydia, kidney and liver damage, diabetes mellitus, vitamin deficiency, exhaustion, endocrine pathology).
- Smoking.
- Decreased protective function of the mucous membranes.
- Living in damp, poorly ventilated and cool areas.
- Living together with the patient.
- Using other people's personal hygiene products (toothbrushes, towels).
- Taking certain medications (cytostatics, immunosuppressants, systemic corticosteroids).

Infection routes
The following routes of penetration of mycobacteria are distinguished:
- airborne (with sputum particles when coughing and sneezing);
- air-dust;
- contact and household (through household items);
- food (rarely).
In 95% of cases, an aerogenic infection mechanism is observed. The clinical picture of the disease will depend on how the mycobacteria entered the body.
Components of the primary tuberculosis complex
The main components of the complex are:
- lymphadenitis (inflammation and enlargement of regional lymph nodes);
- lymphangitis (damage to lymphatic capillaries and trunks);
- specific inflammatory response.

An important condition for the presence of all elements of inflammation is a decrease in immunity.
Stages of the disease
There are the following stages of the development of the disease:
- Initial. It is characterized by infiltration of the lung tissue.
- Cell decay and seeding.
- Resorption of the focus.
- Induration (calcification).
All phases successively replace each other. It all ends with clinical recovery or the development of complications (the spread of infection throughout the body with the formation of secondary foci).
Pneumonic (lung damage)
At an early stage of the disease, pneumonitis develops. The lung tissue becomes inflamed. The process involves 1 or more segments. Along with the primary focus, there is a zone of perifocal inflammation. It appears against the background of toxic pulmonary edema.
Resorption of infiltrate
This stage begins no earlier than 2-3 months after infection. The infiltrate (zone of tissue compaction) is gradually absorbed.
Compression
After 8-10 months, compression (compaction) of the affected area occurs. Pneumosclerosis (fibrosis) develops. Without treatment, this stage lasts up to six months.

Calcification (salt deposition)
After a year or more, the Ghosn focus is formed. Calcium salts are deposited in tissues. Such an area is clearly visible on an X-ray.
Calcifications are determined both in the lung tissue and in the lymph nodes.
Symptoms of the disease
In most cases, the disease is pulmonary. Less commonly, the intestines (with the food route of infection) and the mucous membranes of the oral cavity are affected. The primary complex is characterized by an acute or subacute course. Often, the disease is latent. According to the clinical picture, the pathology resembles flu or pneumonia.
Important information: Features of the development and course of miliary pulmonary tuberculosis
In children and adolescents
In children under 3 years of age, the disease is most severe. The following symptoms are observed:
- fever up to 39-40 ° C and above;
- dyspnea;
- chest pain;
- paroxysmal cough;
- loss of appetite;
- chills.

In the subacute course of the disease, the temperature is most often subfebrile. Disturbed by cough (dry or productive), severe fatigue, weakness and sweating, mainly at night. Objective signs of the disease in children are:
- swollen lymph nodes;
- heart palpitations;
- drop in blood pressure;
- pallor of the skin;
- weight loss (with a protracted course).
Sometimes the liver enlarges.

Often, this pathology is disguised as pleurisy. In this case, chest pain intensifying during coughing, shallow breathing, low-grade fever, chills and weakness are observed. When the pathological focus is localized in the basal segments of the lungs, an abdominal syndrome sometimes appears. It includes abdominal pain and other manifestations of dyspepsia (digestive disorders). In adolescence, complaints may be absent.
In the event of an adult
In adults, the complex is often asymptomatic. In the acute form, there is a cough (often with viscous, difficult to separate sputum), fever and other signs of intoxication. In weakened people, the disease proceeds as pneumonia.
Types of disease course
The primary complex is subacute, acute, asymptomatic. In the latter case, an important sign of the disease is the positive results of the Mantoux test or Diaskintest.
Identification of the primary tuberculosis complex
Phthisiology identifies the following methods for diagnosing the disease:
- Chest X-ray.
- Laboratory tests (clinical blood and urine tests, biochemical analysis, sputum examination for acid-fast mycobacteria).
- Physical examination. Palpation of the lymph nodes, auscultation and percussion of the lungs are performed. With a common pathological process, dullness of percussion sound and small wheezing are possible. Rigid and vesicular breathing is often determined.
- Screening studies (Mantoux test and Diaskintest).
- Interview. Helps to study the epidemiological history and risk factors for infection. Patients' medical history is thoroughly analyzed.
In doubtful cases, magnetic resonance imaging or computed tomography is performed to clarify the diagnosis.
Laboratory diagnostics
In the acute progressive course of the disease, clinical blood and urine tests are informative. Leukocytosis, a shift of the formula to the left and an acceleration of ESR are often observed. A general urinalysis sometimes reveals the presence of protein. If there is no clinic, then the analyzes will be unchanged. Additionally, a quantiferon test may be required.

A study on mycobacteria is carried out three times. The result is positive only in 5% of cases. The material for research is the patient's sputum. In young children, gastric lavage is taken.
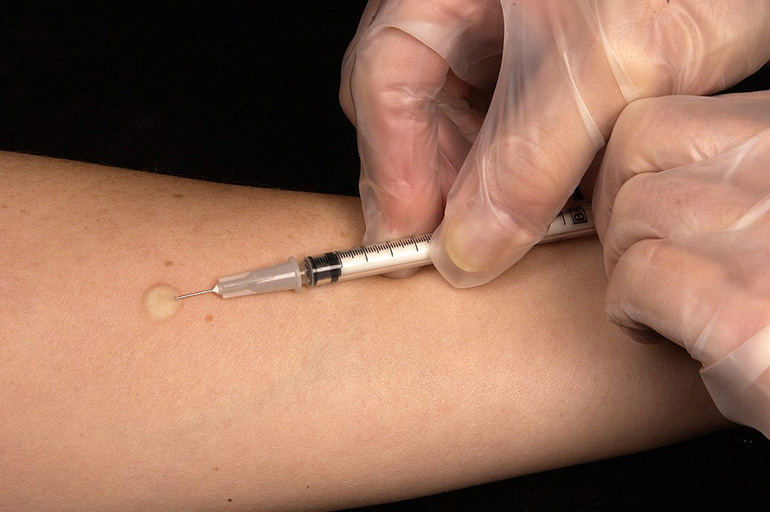
The most informative are the results of immunological analyzes. Characterized by a turn of reactions, when, after previous negative results, a positive one appears. An intradermal injection is performed. The needle is inserted with a cut upward, almost parallel to the skin, into the region of the middle third of the anterior surface of the forearm. A white seal should appear.
The result is assessed by the size of the infiltrate, the presence of redness and vesicular-necrotic changes. With tuberculosis, there are positive (the presence of papules of any size) and hyperergic reactions. In the latter case, the infiltration is more than 15 mm, or there are other signs of the disease (tissue necrosis).
Occasionally, to exclude oncological pathology, a macro specimen (a fragment of lung tissue) obtained during a biopsy is examined.
It is evaluated under a microscope and described.
X-ray
X-ray signs of tuberculosis include:
- The presence of a primary affect. Defined as a shadow up to 1 cm.
- Local decrease in the transparency of the lung tissue.
- Swollen lymph nodes. Better defined in lateral projection.
- Inflammatory pathway from the primary focus to the nodes.
- Hearth of Gona. The light area is rounded with clear contours. The outbreak consists of salt deposits.

The study is carried out in 2 projections: direct and lateral.
Treatment methods
Patients are hospitalized in specialized dispensaries. After recovery, such people should be followed up for 2 years by a doctor. Children with bending reactions and no symptoms of the disease are not hospitalized. The main treatments for tuberculosis are:
- drug therapy (use of chemotherapy drugs, immunomodulators, detoxification agents);
- diet;
- surgical intervention;
- rest in a sanatorium;
- physiotherapy.
Important information: The clinical picture of the course of intestinal tuberculosis in an adult
The main principles of therapy are safety, timeliness, an integrated approach, continuity, duration, constant control and continuity.

An important aspect of treatment is proper nutrition. Patients are shown treatment table No. 11. Nutrition pursues the following tasks:
- strengthening the body;
- increased resistance to infection;
- improvement of metabolic processes;
- restoration of normal energy balance;
- acceleration of the recovery of patients.
You need to eat 4-6 times a day in small portions. The diet should have a protein-carbohydrate orientation. The following foods and dishes are useful:
- raw and boiled vegetables;
- fruits;
- berries;
- greens;
- cereals;
- soups;
- eggs;
- cheese;
- cottage cheese and other dairy products;
- sweets;
- low-fat varieties of fish and meat;
- seafood;
- nuts.

From drinks it is better to use juices, rosehip broth, natural fruit drink, herbal (green) tea and still water.
Surgical intervention
Surgery for tuberculosis is rarely required. In advanced cases, with residual effects after drug therapy and with the transition of the disease to a secondary form, the following interventions are possible:
- resection (removal of part of the lung);
- cavernotomy (removal of a cavity with decaying tissue);
- pleurectomy (removal of part of the pleura);
- thoracoplasty.
After surgery, pain relief, anti-tuberculosis drugs, regular dressings, adherence to bed rest, physical and mental rest, control X-ray study.

Chemotherapy use
Tuberculosis is a curable disease. The goal of drug therapy is to destroy mycobacteria in the body. Medicines must be broad-spectrum and effective against the infectious agent. The choice of drugs is carried out taking into account the allergic history and the age of the patients.
In the treatment of tuberculosis, chemotherapy drugs of the 1st line are used. 4-5 drugs can be prescribed at the same time. These include:
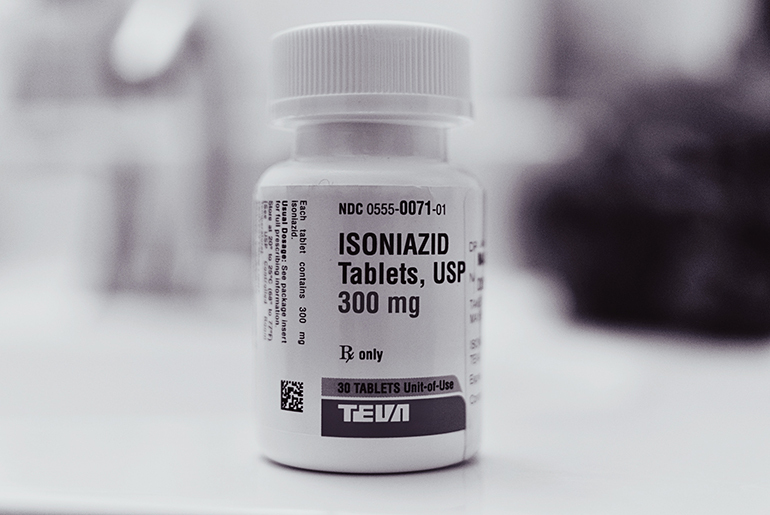
- Isoniazid. One of the most effective remedies. It is used in the form of tablets and solution for injection. Has a bactericidal effect (kills germs). It is used in the treatment of all types of tuberculosis. Contraindicated in case of intolerance, drug-induced hepatitis, severe liver failure and children under 3 years of age (tablets). It is prescribed with caution for alcohol addiction, seizures, HIV infection, diabetes, hypothyroidism and mental disorders.
- Rifampicin (Rimpin, Rifampicin-Ferein). Forms of release - capsules for oral administration and lyophilisate (powder for solution for injection). Acts bactericidal by disrupting the synthesis of RNA of microbial cells. The pathogen quickly becomes resistant to rifampicin, so it is used in combination with other drugs. The drug is not prescribed for jaundice, renal dysfunction, hepatitis and intolerance.
- Pyrazinamide. A synthetic agent that penetrates well into tissues and kills mycobacteria. Release form - tablets for oral administration. Contraindications include hypersensitivity and liver failure. Side effects are possible in the form of indigestion, rash and itching.
- Ethambutol (Etumbusin). Used in pill form. Acts on typical and atypical pathogens of tuberculosis. Able to penetrate cells. It is prescribed for pulmonary and extrapulmonary tuberculosis. Contraindications include cataracts, retinopathy with diabetes, neuritis, gout, eye diseases, severe renal dysfunction, age up to 13 years, pregnancy and lactation. The dosage is determined by the doctor taking into account the patient's weight.
- Streptomycin (powder). An antibiotic from the aminoglycoside group. It is prescribed for tuberculosis of the lungs and other organs. A solution is prepared from the powder, which is injected intramuscularly or through the trachea. The drug has a nephrotoxic effect. Contraindicated in pregnant and lactating women.
Less commonly, second-line drugs are used (Ethionamide, Cycloserine, Kanamycin, Ofloxacin, Capreomycin, Levofloxacin, Terizidone). Combination drugs are often prescribed. They contain several antibiotics at once, which does not require the use of a large number of tablets. These drugs include:
- Repin B6 and its analogues (Laslonvita, Izokomb, Protub-4 Plus). Contains vitamin B6 (pyridoxine), isoniazid, ethambutol, pyrazinamide and rifampicin. Available in pill form. Contraindicated in exacerbation of diseases of the gastrointestinal tract, CNS pathology, optic neuritis, retinopathy, pregnant women, lactating women and children under 13 years of age.
- Phyzoetam. The active ingredients are isoniazid and ethambutol. Appointed from the age of 12. Contraindicated in eye diseases, arterial hypertension, myxedema, liver dysfunction, epilepsy, gout, psoriasis, ulcers, coronary insufficiency, pregnant and lactating.
- Combitub. It contains rifampicin, ethambutol, isoniazid and pyrazinamide. It is not prescribed for kidney and liver pathology, thrombophlebitis, epilepsy, seizures, atherosclerosis, visual impairment and intolerance. Suitable for patients over 13 years old.
- Rifakomb (Tubavit). The active substances are rifampicin and isoniazid. The auxiliary component is pyridoxine. It is administered orally. Contraindications are impaired renal function, jaundice, infancy, pregnancy and lactation.
- Lomecombe. Contains levofloxacin, ethambutol, isoniazid, pyrazinamide and pyridoxine. It is taken orally regardless of food. Suitable for adults only.
- Phthisopyram. The active ingredients are isoniazid and pyrazinamide. Effective in all forms of tuberculosis. It is not prescribed for asthma, myxedema, psoriasis, gout, high blood pressure, hyperuricemia, ulcers, heart failure, cirrhosis, hepatitis and epilepsy.
The average duration of drug treatment is 3 months.
Bronchial block (valve installation)
If a cavity of tissue decay is formed in the lung, bronchoblocking may be required. This is an invasive procedure that involves the placement of a special valve. It creates hypoventilation in the affected area, which helps to close the decay cavity. At the same time, the drainage function is preserved (sputum is released freely).
Important information: The clinical picture of the development of tuberculous pleurisy in humans

Such an intervention is indicated in the transition of primary tuberculosis to more severe forms with tissue destruction.
Recovery period
During the period of recovery of lung function, it is recommended:
- physiotherapy;
- rest in a sanatorium or dispensary;
- taking vitamin complexes (Vitrum, Supradina);
- good nutrition, enriched with vegetables and fruits;
- to give up smoking;
- elimination of stressful situations and hypothermia;
- temporary refusal from planned operations (except for vital ones);
- refusal to administer vaccines.

For those who have had tuberculosis, dispensary observation is established.
Complications and consequences
If the treatment was provided out of time or incompletely, then the following complications are possible:
- Severe pulmonary fibrosis. Functional (airy) tissue is replaced by coarse connective tissue, resulting in respiratory failure.
- Development of secondary forms of tuberculosis (focal, disseminated, miliary, cavernous, infiltrative, cirrhotic, fibro-cavernous).
- Severe tissue breakdown (cirrhosis).
- Bleeding.
- Hemoptysis.
- Fistula formation.
- Dissemination (spread) of mycobacteria throughout the body with damage to other organs and systems (intestines, eyes, skin, bones, joints, bladder, pleura).
- Meningitis. It is characterized by inflammation of the meninges. Manifested by severe headache, nausea, irritability, high fever, increased sensitivity to light and sound, meningeal symptoms, confusion and lethargy.

Prevention for the risk group
Prevention of tuberculosis is specific and non-specific. It starts at an early age to reduce the risk of contracting mycobacteria and to ease the progression of the disease.
Primary measures
Primary preventive measures include:
- Vaccination. The drug BCG or BCG-m is used (sparing for sensitive people). They contain live, weakened infectious agents. The release form is a lyophilisate for obtaining a solution for intradermal administration. Vaccination against tuberculosis is included in the list of vaccinations on the national calendar. Injections are given in the first week of life and 6-7 years. Contraindications to vaccination include prematurity, acute inflammatory and infectious diseases, cancer, and primary immunodeficiency.
- Regular tuberculin diagnostics. The Mantoux test and Diaskintest are used. Conducted in kindergartens and schools.
- Fluorography. Should be held every year.
- Increasing the body's resistance (good nutrition, taking vitamins, playing sports, giving up bad habits).
- Exclusion of contact with the source of infection (sick person).
- Timely identification of the sick.
Secondary activities
Secondary prevention means:
- timely treatment of the underlying disease in order to prevent complications;
- early access to a phthisiatrician or therapist;
- dynamic observation;
- careful use of medications;
- consistent improvement;
- periodic inspections.
This is an incomplete list of activities. To reduce the risk of infection for contact and people living with the sick person, it is necessary:
- isolate the source of infection;
- disinfect the premises and household items;
- allocate utensils for each family member.
These measures are required in the development of more severe forms of tuberculosis, when a person releases mycobacteria into the environment with sputum.
Useful materials
Tuberculosis is curable. The prognosis with timely therapy is relatively favorable. To prevent this dangerous disease, it is recommended that you familiarize yourself with the materials on vaccination of children, the benefits of vaccinations and all kinds of risks. It is also helpful to be aware of non-specific infection prevention measures.