Content
- General information about the disease
- Disease code according to ICD-10
- Detailed pathogenesis
- Bone tuberculosis infection routes
- Classification by lesions
- Other provoking factors
- The first signs and symptoms
- By the focus of the lesion (table)
- General clinical picture
- Are there any differences between children and adolescents
- More about spinal tuberculosis
- About tuberculous damage to the joints
- Rare forms of the disease
- Spina ventosa tuberculosa
- Cavernous tuberculous osteitis
- Ponce's disease
- Still-Shoffard disease
- Features of the course in children
- Diagnosis of bone tuberculosis
- Examination and history taking
- Clinical activities
- Radiography
- Laboratory tests
- Standard treatments
- Chemotherapy
- Surgical intervention
- Orthopedic aids
- Abscessctomy procedure
- Physiotherapy
- Complex exercise therapy
- Sanatorium treatment
- Traditional medicine for relief
- Possible complications
- Patient prognosis
Today, the incidence rate of bone tuberculosis is more than 20% in relation to other localizations of tuberculosis infection. Difficulties in early diagnosis and an increase in cases of infection with resistant strains of the pathogen increase the risk of patient disability.

General information about the disease
Osteoarticular tuberculosis is an infectious disease caused by mycobacteria (MBT) belonging to the so-called. group of the tuberculosis complex. The tubercle bacillus has a number of features.
It belongs to the group of acid-resistant pathogens and tends to mutate, which determines its ability to form strains resistant to antibiotic therapy.
Disease code according to ICD-10
According to the international classification of diseases (ICD-10), tuberculosis of bones and joints has a code A 18.0+ "Tuberculosis of other organs".
Detailed pathogenesis
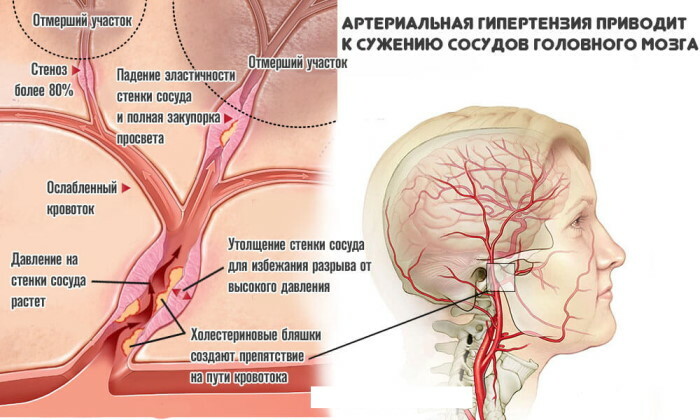
Bone tuberculosis is caused by a secondary infection. With airborne droplets, an infectious agent is transmitted from a patient to a healthy person and settles in the lower lobes of the lungs and alveoli. In the presence of appropriate endogenous conditions, a primary focus is formed there. It is small, limited, and prone to calcification.
From the focus of infection in the lungs, MBT with blood or lymph flow enters:
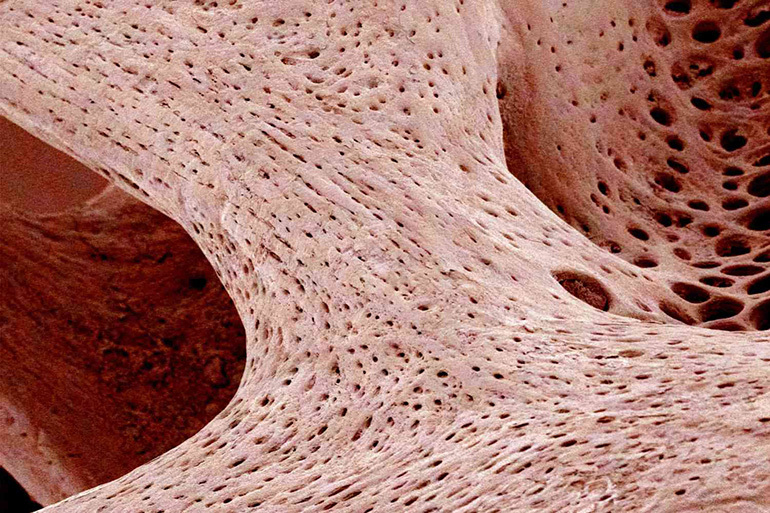
- cancellous bone tissue;
- epiphyses of the femur, humerus;
- the head of the bones of the lower leg, forearm;
- vertebrae, because they are abundantly penetrated by blood vessels.
In the bone tissue, under the influence of the multiplying MBT, an inflammatory process occurs and granulomas - tubercles are formed. They are rarely solitary. With the progression of inflammation and active reproduction of the pathogen merge, forming the so-called. conglomerate tubercle that looks like grayish nodules gathered in clusters. Conglomerates are surrounded by granulations. The alternation of the latter and tubercles is characteristic of the normal tissue reaction in response to the introduction of a pathogen.
However, an atypical tissue reaction is often observed, in which the following are noted:
- proliferation of connective tissue with a small amount of granulomas (fibrous form);
- overgrowth of unstable, bleeding granulomas with a small amount (fungus).
Fungous form is especially characteristic of tuberculous lesions of the synovial membrane of the joints.
Caseous (cheesy) tissue decay can begin inside the tubercle and gradually spread to adjacent tissues. Under favorable conditions, there is an overgrowth of the necrosis focus with strong connective tissue and even its scarring. The process may be accompanied by the loss of calcium salts - calcification.
Under unfavorable conditions, the pathological process continues to capture new tissue areas. When necrotic masses are isolated from fistulas, tuberculosis is contagious. Exudative changes occur around the focus of caseous necrosis: fluid effusion into the surrounding areas, the formation of edema and the development of a new site of inflammation.
In such cases, inside the focus, there is often a disintegration of the contents and destruction of tissues with the formation of cavities - caverns. The addition of pyogenic bacteria enhances suppuration and destruction. When the infection spreads, periarticular and articular elements are captured.
Bone tuberculosis infection routes
Routes of primary infection with mycobacteria:
- Aerogenic (air, inhalation) - the ingress of bacteria into the respiratory tract of a healthy person occurs during his close contact with an infected person.
- Alimentary (food or enteral) - the pathogen enters the digestive system with contaminated food: milk, meat.
- Pharyngo-oral (mixed) - MBT immediately falls on the mucous membrane of the mouth and nasopharynx. This route of infection leads to infection of the cervical lymph nodes.
- Cutaneous (cutaneous) - through the damaged epidermis, the office immediately enters the lymphatic system.

Intrauterine infection is rare. It is possible only with pathology of the structure of the placenta.
Lymphogenous and contact pathways of infection are more common in tuberculosis of the bones of the thoracic skeleton. The ribs, vertebrae, directly in contact with the focus in the lungs, are damaged.
At the same time, the spread of the process from the outside of the bone to the inside is noted, and with hematogenous, on the contrary, from the inside to the outside.
Classification by lesions
Depending on the location of the pathological focus, tuberculosis is distinguished:
- The spine (spondylitis) is one of the most severe forms, mainly the vertebral bodies are affected and, less often, the arches, spinous processes.
- Knees (drives) - manifests itself more often in adolescents, since large bones are most vulnerable during growth.
- The hip joint (coxitis) - also often found in children, leads to deformation and shortening of the lower limb.
- Ankle and foot - accompanied by the formation of fistulas, fusion of the articular surfaces (ankylosis).
- Shoulder.
- Wrists.
- Elbow - rare.
- Tubular bones - damage to the bone itself is rare, since inside there is a yellow bone marrow, the resistance of which to infectious agents is higher than that of red bone marrow.
Other provoking factors
The immunobiological factor is decisive. It determines not only the occurrence of a secondary process in the osteoarticular apparatus, but also the characteristics of the course of the disease. Heredity plays a minor role. There is no evidence of a familial predisposition to this pathology.

Other reasons:
- excessive physical activity;
- cooling microclimate;
- stress and neuropsychiatric disorders;
- joint and bone injuries;
- unfavorable socio-economic living conditions;
- exhaustion, unbalanced nutrition;
- addiction (drug, alcohol);
- chronic infectious pathologies;
- increased sensitization of the body to the pathogen;
- pathological reaction to vaccination.
The first signs and symptoms
Symptoms depend on the stage of the disease. At the initial stage, a focus of inflammation occurs in the red bone marrow in the area adjacent to the epiphyseal plate. There are no clinical manifestations at this stage. The first signs of the disease:
- mild pain;
- slight lameness;
- lack of radiological signs.

The arthric phase is characterized by an increase in local symptoms:
- joint pain that gets worse during movement;
- an increase in the volume of the joint;
- smoothing the contours of the articulation;
- muscle atrophy of the lower extremities or shoulder girdle;
- hypertrophy of subcutaneous fat.
At this stage, general and radiological signs are enhanced.
In the post-arthric phase, inflammation subsides and the symptoms accompanying the pathology disappear. Complications are noted:
- ankylosis;
- joint contractures;
- non-physiological position of the limb;
- functional disorders.
Important information: The clinical picture of the development of cavernous pulmonary tuberculosis in adults
By the focus of the lesion (table)
The following table shows signs of pathology in different phases and with different locations of the lesion:
| Localization of the focus | Phases of the pathological process and the corresponding signs | ||
| Initial | High | Attenuation | |
| Vertebral column |
|
|
|
| Hip joint |
|
|
|
| Knee |
|
|
|
| Ankle and foot |
|
|
|
| Shoulder joint |
|
|
|
| Wrist and hand bones |
|
|
|
General clinical picture
Analyzing the manifestations of pathology, one can note general symptoms at the corresponding stages of development. Not only the local manifestations listed in the table are similar, but also the signs of general sensitization of the body:
- increased weakness;
- dizziness;
- nausea, vomiting;
- fast fatiguability;
- decreased performance;
- loss of appetite;
- restless sleep (especially in children);
- subfebrile temperature, which periodically rises to febrile;
- excessive sweating.

If at the initial stage signs of intoxication are minimal or absent, at the height of the pathological process they become pronounced, and in the final phase they subside again.
Are there any differences between children and adolescents
In children, the disease progresses with more severe symptoms and severe consequences. This feature is due to the immaturity of the bone and nervous systems.
Large lesions are found in the growth zones of the bones, the cartilage tissue of the joints degrades much faster, which leads to ankylosis. If the pathology in adults can be cured without surgery, a small child and adolescent needs surgery to avoid complications. After prompt removal of the affected lesion, all of the above violations disappear:
- muscle tone and volume are restored;
- demineralized and destructive areas are compacted, the architecture of the bone is restored;
- the inhibition of longitudinal bone growth stops.
Necrotic and dystrophic changes disrupt bone growth and lead to skeletal, posture, and limb anomalies. Large tubular bones become shorter and thinner. With tuberculous drive and coxitis, the growth retardation of the limb can be 15-20 cm. This is typical not only for the affected bones, but also for others that are far from the focus.
Tuberculosis infection suppresses the functions of all growth zones of the limb. Children have a higher risk of disability and irreversible skeletal changes.
More about spinal tuberculosis
This is one of the most common and most common types of pathology. This phenomenon is due to the structure of the spinal column and its role in maintaining an upright posture, ensuring motor function.

Inflammation (spondylitis) begins in the spongy substance of the vertebral body and rarely in the spinous processes and arches, since they are similar in structure to flat bones. The process can involve from 1 to 3 vertebrae. As the disease progresses, up to 10 segments of the spine can undergo changes.
The disease leads to softening and weakening of the vertebra. Under the pressure of the overlying sections, wedge-shaped deformation of the vertebral body and compression of the nucleus pulposus, intervertebral discs, and nerve endings occur.
With the progression of the pathology, inflammation passes to the adjacent sections and tissues:
- the spinal cord, which causes neurological disorders (paresis, paralysis, disruption of the pelvic organs);
- nucleus pulposus and intervertebral discs, with a decrease in the height of the spine and its curvature;
- adjacent soft tissues, in which drip abscesses are often formed, a secondary infection may join and fistulas may appear.
Small intervertebral joints are rarely involved in the pathological process. In them, degenerative changes most often occur, which lead to loss of mobility of the spine - ankylosing spondyloarthrosis.
Complications after elimination of active inflammation are severe.
Paralysis, irreversible curvature of the vertebral sections, hump, deformity of the chest, twisting and skewing of the pelvis may develop.
About tuberculous damage to the joints
Most often, large tubular bones are infected. In their periarticular heads there is a red spongy tissue, into which Koch's sticks are brought in by the blood stream. Inflammation is accompanied by the formation of tubercles, merging into conglomerates. Caseous necrosis occurs inside the formations.
Important information: The clinical picture of the development of focal pulmonary tuberculosis

Gradually, the inflammation spreads to the joints. Pathology covers the synovium. As a result of inflammation, an effusion occurs into the articular cavity, the articulation is deformed, mobility decreases, and soft tissue edema develops.
Inflammation, which lasts for a long time and slowly in the bone in a latent form, becomes more aggressive during the transition to the synovium. This is due to the structure and trophism of different tissues. The articular membrane reacts violently to the influence of an infectious agent. The processes of proliferation and caseous necrosis are actively proceeding in it. Inflammation of the membrane also leads to early osteoporosis, which increases the incidence of fractures of the affected bones.
The joint cavity is filled with a small amount of elastic, dense fluid. It provides nourishment to the cartilage in which there are no blood vessels. Therefore, the liquid is an excellent breeding ground for the reproduction of MBT. Tuberculous arthritis occurs.
Due to the lack of microcirculation, the cartilage of the articular surfaces resists the impact of pathogen, but with the prolonged presence of an effusion in which toxic substances are formed, it begins degrade. There is a decrease in the joint space, the head of the bone is exposed. The most dangerous complication of pathology is the fusion of surfaces (ankylosis). The joint loses mobility, and the limb takes a non-physiological position.
For example, tuberculosis of the knee joint (the symptoms were described above) leads to disability, loss of limb mobility.
Fistulas are often formed in the popliteal fossa. In children, there is a growth retardation of the limb, curvature of the spine, twisting of the pelvis.
Rare forms of the disease
In addition to the listed forms of the disease, pathogenic processes are also noted in other parts of the skeleton. They develop much less frequently and account for about 3% of all cases of tuberculosis infection.
Spina ventosa tuberculosa
Bone shaft tuberculosis is diagnosed in children. The low incidence of pathology with such localization is explained by the properties of the tissue filling the tubular bone. The yellow bone marrow tissue is composed of fat cells and has a weak circulatory system.

Most often, the small bones of the foot and hand are affected. Less commonly, long limbs. The process follows the same principle as in other parts of the tissue. But if in the pineal glands it is directed from the inside out, with damage to the middle part of the bone, it affects the periosteum and tends inward. The beam structure of the tissue is destroyed, and early osteoporosis develops. With the spread of inflammation to soft tissues, the formation of drip abscesses and fistulas occurs.
Cavernous tuberculous osteitis
The disease most often affects adolescents during puberty. The pathological process covers the small bones of the hands and feet. Jungling's cystic osteitis proceeds in a benign form: there is no caseous necrosis, the architectonics of the bone is preserved, there are no large foci of dead tissue.
Pathology can be localized in other parts of the skeleton: vertebrae, bones of the skull or pelvis. But such an arrangement of foci is not typical for this form of the disease.
Jungling's tuberculous osteitis has 3 forms:
- There are small cysts in the bone tissue, the function of the limb is preserved.
- There are gross changes in the structure of the tissue. The cellular part is almost completely replaced by cysts.
- Destruction covers all types of tissues, bone destruction (osteolysis) occurs. Frequent fractures, severe deformity, and dysfunction are noted.
With the defeat of the phalanges of the fingers, their swelling, redness is observed.
The patient looks and feels like a frostbite of a limb. Some consider the disease to be a bone form of sarcoidosis.
Ponce's disease
The disease has similarities in clinical manifestations, radiological picture and morphological signs with those in rheumatoid arthritis. Pathology occurs with the same frequency in men and women. The average age of patients is 28-30 years. Large articular joints of the skeleton are affected. The number can vary from 2 to 4 joints. The disease is difficult to identify and differentiate. Therefore, it is often confused with rheumatoid arthritis.

It is assumed that the cause of the development of pathology is an allergic reaction to MBT. Moreover, the focus of infection may not be located in the bone tissue and be in a latent state. Antirheumatoid therapy is ineffective. Treatment of patients with anti-TB drugs leads to rapid resolution of arthritis. With prolonged absence of adequate treatment, ankylosis of the joint can occur.
Still-Shoffard disease
The disease is rare. The frequency of occurrence is 1 person per 100 thousand. It is equally often diagnosed in women and men. Until recently, it was believed that the disease affects only children and adolescents under 16 years of age. But in the 70s. XX century numerous cases have been described in adults.
Pathology proceeds with the following manifestations:
- severe fever;
- rashes on the skin;
- polyarthritis;
- inflammation of internal organs.
Symptoms indicate the infectious nature of the pathology, but a single pathogen has not yet been identified.
Therefore, disputes about the belonging of this disease to the forms of bone tuberculosis are still ongoing.
Features of the course in children
Pathology is diagnosed in children during the first 5 years of life. Then the incidence rate decreases and becomes a minimum by the age of 20. This is due to the rapid growth of the skeleton, the formation of bone tissue and the immaturity of the immune system.

In children, the disease is more acute. The general symptoms of pathology are expressed, which indicates a strong intoxication of the whole organism. Local manifestations are also pronounced. Pathology is accompanied by a rapid increase in degenerative-dystrophic changes. Even after the resolution of the acute process, irreversible structural and functional disorders remain.
Diagnosis of bone tuberculosis
TB is difficult to diagnose, especially in the early stages of development. Comprehensive diagnostics is required, including the following research methods:
- clinical;
- radiological;
- laboratory.
To determine some forms of pathology, a differential diagnosis is required.
Examination and history taking
The initial stage of diagnosis is visual, physical examinations and collection of anamnesis. Doctor:
- finds out the presence of contacts with a patient with tuberculosis;
- conducts Mantoux tests;
- with an extrapulmonary form, prescribes a more informative study - the Koch test;
- establishes a history of infectious diseases;
- studies the epidemiological environment;
- evaluates the symptoms of general intoxication;
- finds out the time of occurrence of signs of pathology.

The specialist examines and measures the limbs, reveals shortening, volume reduction, muscle stiffness and joint stiffness.
Clinical activities
To establish the clinical picture of the disease, the doctor not only conducts a conversation with the patient, but also prescribes a series of tests to identify impaired motor function, the state of the joint and muscles. Recommends to undergo a complete blood count, which helps to identify the presence of inflammation in the body. For research, take urine and sputum.
Important information: Features of the manifestation of genital tuberculosis in men and women
Radiography
X-ray and some radiation research methods are basic in the detection of bone tuberculosis. These methods make it possible to see not only violations of the tissue structure, but also to trace the dynamics of the process.

Radiography makes it possible to identify osteoporosis, bone deformation, foci of destruction, sequestration, the state of the articular elements. An experienced specialist may notice the presence of drip abscesses.
In-depth methods of X-ray diagnostics - CT, MRI, allowing timely detection of destructive changes that are not detected by standard X-ray research.
Laboratory tests
Laboratory studies help to identify pathology at the initial stage, when structural changes are still absent. They allow you to track the effectiveness of treatment and timely correct it. Laboratory research methods used to confirm the diagnosis:
- biochemical - blood serum, synovial fluid, joint contents, abscess are examined;
- cytological and histological analyzes of biopsy material;
- PCR;
- ELISA.
These methods make it possible to identify not only the presence of MBT, but also their number, phase of activity, virulence.

In addition, additional survey methods are used:
- arthrography;
- myelography;
- spondylography;
- abscessography.
Only when using a complex of techniques can an accurate diagnosis be made at an early stage.
Standard treatments
Treatment standards include specific and non-specific treatments. The first are:
- symptomatic therapy;
- chemotherapy;
- surgical intervention;
- use of orthopedic aids.
Non-specific therapy methods include:
- good balanced nutrition;
- vitamin therapy;
- Exercise therapy;
- heliotherapy;
- aerotherapy;
- Spa treatment.

Complex treatment takes a long time - from 1.5 to 3 years.
Chemotherapy
When carrying out chemotherapeutic treatment, antibacterial drugs of a wide spectrum of action and anti-tuberculosis drugs are used:
- Tubazid;
- Ortivazide;
- Larusan;
- Satozide;
- Kanamycin;
- Rifampicin;
- Isoniazid;
- Ethambutol.
The regimens (combination of drugs and duration) of chemotherapy are determined by the attending physician based on the drug sensitivity / resistance of mycobacteria and the effectiveness of treatment.

With the low effectiveness of the drugs of the main group, the means of the second are used:
- PASK;
- Ethionamide;
- Propionamide;
- Terizidone;
- Pyrazinamide.
Treatment can be supplemented with hormonal agents. When establishing active tuberculous arthritis or spondylitis, a combination of 4-5 anti-tuberculosis drugs with a total duration of up to 8-10 months, followed by seasonal preventive courses.
Surgical intervention
It is indicated to treat pathology with the help of surgical methods if chemotherapy does not give a pronounced effect and there is an increase in gross changes in bones and joints. At different stages, specific methods of surgical treatment are used:
- Radical - to remove a necrotic focus: necrectomy, articular resection, extra-articular bone resection, extra-articular arthrodesis, synovectomy, abscessotomy, osteoplasty, limb amputation.
- Corrective and reconstructive: osteotomy, arthroplasty, alloplasty, osteoplastic fixation of the spine, prosthetics.

After applying conservative or surgical treatment, proceed to the next stage.
Orthopedic aids
These treatments include:
- immobilization with a plaster cast;
- bed rest;
- traction of a limb or spinal column;
- wearing a plaster or removable corset (after the active phase subsides);
- the use of orthoses for diseases of the lower extremities;
- the use of extrafocal compression-distraction devices, splints.
For the immobilization of young children, special plaster beds are used, which are changed every 3-4 months. Orthopedic means are shown during the deformity period, to maintain the statics of the limb and spine.

Abscessctomy procedure
In order to remove the contents of the abscess and affected tissues, an operation is performed - an abscessctomy. First, the abscess is emptied through a puncture needle, then an aqueous dye is injected into its cavity - a solution of blue, brilliant green. Radical removal involves the excision of all tissue stained with this. The area of the removed abscess is tamponed or drained with tubes.
Physiotherapy
In the recovery period after surgery and drug therapy, physiotherapeutic methods are prescribed:
- electrophoresis with drugs;
- phonophoresis;
- UHF therapy;
- amplipulse therapy;
- phototherapy;
- magnetotherapy.
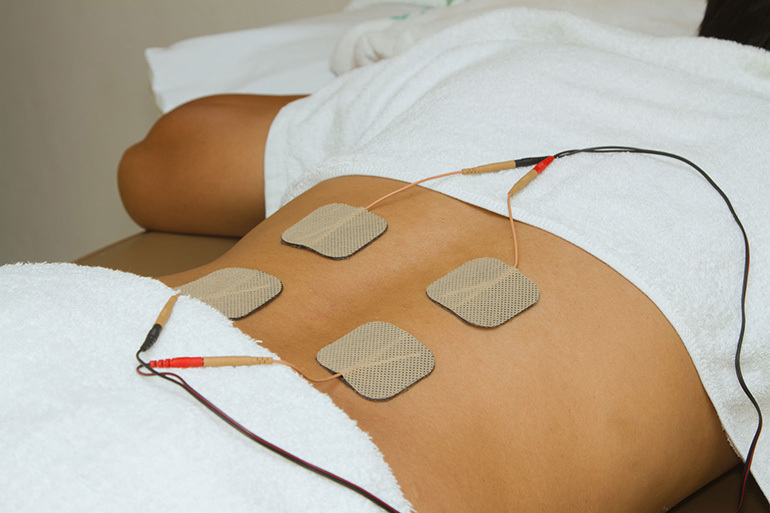
The duration of the procedures and the number of sessions are determined by the attending physician.
Complex exercise therapy
Physiotherapy helps to restore the functions of the affected limbs and spine, to strengthen muscle corset, normalize muscle tone, activate microcirculation in tissues and speed up processes regeneration. A set of exercises is developed by a rehabilitation doctor.
Sanatorium treatment
Tuberculosis sanatoriums are located both in the patient's places of residence and in resort areas. People can be sent to local sanatoriums after elimination of symptoms of acute intoxication and with signs of stabilization of the process.
The second phase of chemotherapy in local sanatoriums is preferable for older age groups, young children and patients after surgery for tuberculosis. People who can be expected to have a more complete involution of lesions in a short time are sent to resort sanatoriums.

Traditional medicine for relief
Folk remedies are used in the complex treatment of the disease and during the recovery period. Medicinal plants are used:
- roots of yellow water lilies - for preparing warm baths to relieve pain;
- a mixture of aloe juice with lard, honey and cocoa - for internal use;
- Bolotov's kvass - to eliminate intoxication.
To increase immunity and activate the processes of self-healing of the body, beekeeping products are used: tincture of wax moth or beesworm, honey with royal jelly.
Possible complications
Even when the active process subsides, reversible and irreversible complications can occur:
- scoliosis, hump;
- fistulas and abscesses;
- joint stiffness;
- paralysis;
- contractures;
- spinal stenosis;
- muscle atony;
- deformation of the chest;
- displacement and dysfunction of internal organs.
Some complications can be corrected surgically. Certain types of pathologies are capable of self-regression.
Patient prognosis
With early detection and adequate treatment, a positive result of therapy is achieved in 99% of cases. In 66%, with the use of non-radical treatment, there is a chronicity of the process and relapses of the disease.
With a frequency of 3-30% of cases with radical therapy, there is a shortening and deformation of the limbs for a period of 4-12 years after the operation. With tuberculous arthritis, functional disorders develop in almost ½ cases.