Arterial hypotension exposed to a large number of people around the world. There are several forms of hypotension. One of them is orthostatic hypotension. This phenomenon is a decrease in blood pressure.
Record content:
- 1 What it is
- 2 Varieties
- 3 Causes
- 4 Symptoms
- 5 First aid
- 6 Drug treatment
- 7 Recommended diet
- 8 Complications and consequences
- 9 Disease video
What it is
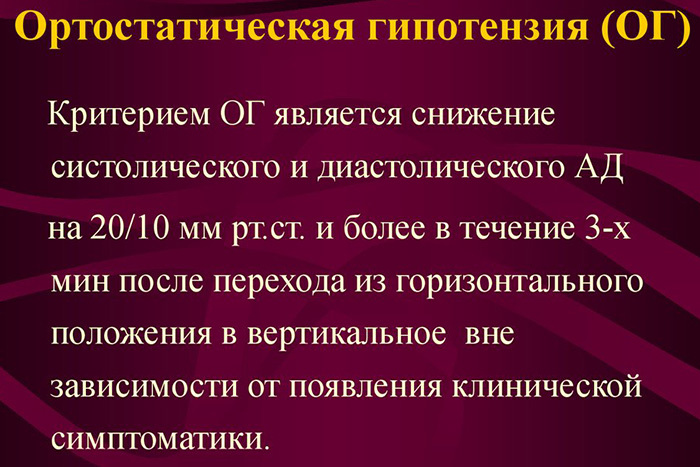
Orthostatic hypotension - This is a pathological condition characterized by a sharp decrease in blood pressure by more than 10 mm. rt. Art. with a sharp rise from a horizontal position to a vertical one. With this type of hypotension, both indicators, diastolic and systolic pressure, and one of them decrease.
In another way, orthostatic hypotension is called postural. This type of pathology is not an independent disease, but has the character of a symptom of one of the pathological conditions.

People of both sexes are susceptible to orthostatic hypotension, but this pathology is more common in women.
The age of development of this phenomenon fluctuates in the region of 40-45 years. Although there are options for the development of hypotension in young people. Most of all, people with chronic vascular and nervous system disease, as well as patients with long-term arterial hypertension, are susceptible to this.In elderly and senile people, hypotension is diagnosed in 30% of cases, and the vast majority of cases remain diagnosed, since in elderly people, orthostatic hypotension occurs in the form of short-term episodes of loss consciousness.
The pathogenesis of pathology consists in violations of the body's mechanisms that are responsible for the regulation of blood pressure.
Varieties
One of the varieties of orthostatic hypotension is postural orthostatic tachycardia syndrome. This phenomenon occurs in younger patients and is an increase in pulse rate (more than 120 beats per minute) when changing position from horizontal to vertical. At the same time, a slight decrease in blood pressure is also observed.
Orthostatic hypotension is a pathology that is divided into several distinct forms:
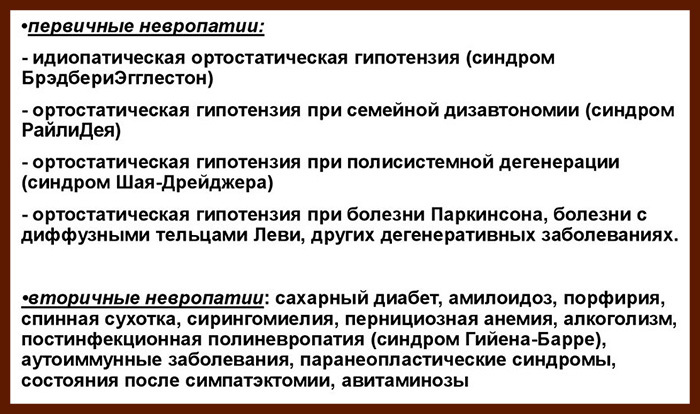
- Neurological form. It occurs in the vast majority of cases of hypotension. The incidence is approximately 70% of all reported cases. This form is an independent nosological unit. The mechanism of development of the neurological form consists in disruption of the sympathetic and parasympathetic nervous systems.
- Idiopathic form. The idiopathic form is considered a diagnosis of exclusion when the cause of the pathology is unknown.
- Medicinal orthostatic hypotension. It develops against the background of taking diuretics, nitroglycerin, calcium antagonists and drugs for the treatment of arterial hypertension. When taking these medications, vasodilation occurs, the load on the heart decreases, and the osmotic pressure decreases. All this leads to a sharp drop in blood pressure. Drug hypotension is treated by discontinuing the drug that caused orthostatic hypotension. In addition, it is possible to adjust the dose of the drug.
- Shai-Drager syndrome (multisystem atrophy). This disease is relatively rare. It is a lesion of the nervous system and a violation of the production of norepinephrine. As a result, the vasoconstrictor effect is disrupted in the body.
- Hypovolemic orthostatic hypotension. It occurs when the body is dehydrated from massive bleeding, loss of fluid. This form is observed in acute or chronic bleeding, during trauma, childbirth, decay of tumors and other pathologies. And also hypovolemia develops with hyperthermia (fever), infectious diseases, mainly intestinal. Intestinal infections (dysentery, cholera) are accompanied by rapid dehydration, which can lead to such a phenomenon as orthostatic hypotension.
According to its course, orthostatic hypotension is divided into primary and secondary:
- Primary. It is diagnosed as an independent disorder in the functioning of the nervous system or a form without an established cause. And also the primary dosage form of orthostatic hypotension can be attributed.
- Secondary. It develops as a result of any disease. As an example, this is myocardial infarction, the consequences after a stroke.
Causes
Pathological changes in the nervous system against the background of diseases can lead to disturbances in the mechanisms responsible for maintaining normal blood pressure levels.
Episodes of a sharp drop in blood pressure can be caused by many reasons:
| Causes | Examples of diseases |
| Diseases of the central nervous system | Consequences after multiple stroke (ischemic, hemorrhagic), multisystem atrophy, Parkinson's disease, multiple sclerosis. |
| Infectious diseases | Severe bacterial and viral infections (influenza, pneumonia), meningitis, meningoencephalitis, tuberculosis, sepsis. A special role is assigned to the occurrence of intestinal infections and the development of dehydration. |
| Inadequate intake of B vitamins, potassium and sodium | Avitaminosis, malnutrition, sudden weight loss, anorexia and cancer cachexia. |
| Oncological processes | Tumors of the nervous system and brain. Orthostatic hypotension can also occur during metastasis and during chemotherapy (as a side effect). |
| Brain tumors | A separate group is brain neoplasms (gliomas, adenomas). Their growth provokes pressure on important functional areas, due to which false signals are transmitted along the nerve pathways. |
| Peripheral Nervous System Disorders | Vegetovascular dystonia (VVD) or hypotensive neurocirculatory asthenia, amyloidosis, pareneoplastic syndromes, Guillain-Barré syndrome. |
| Hypovolemia | Dehydration (dehydration), bleeding. Blood loss can be both acute and chronic (from internal organs). |
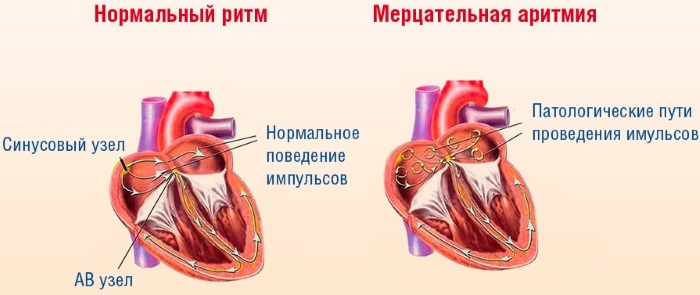
| Pathology of the cardiovascular system | Myocardial infarction, heart failure, aortic stenosis, cardiac arrhythmias, pericarditis, heart defects, severe mitral valve prolapse, PE (pulmonary embolism). |
| Violations of vascular tone | Hypokalemia (lack of potassium in the body), prolonged bed rest. |
| Benign Brain Tumors | Pheochromocytoma |
| Vein pathology | Chronic venous insufficiency |
| Spinal cord pathology | Tumors, myelitis (inflammation of the spinal cord). |
| Hormonal Disorders | Adrenal insufficiency, diseases of the reproductive system. In addition, type 1 diabetes mellitus, thyroid pathology (hypothyroidism) are isolated. |
| Postprandial orthostatic hypotension | A sharp release of insulin after eating or with diseases of the gastrointestinal tract. |
| Physiological processes | Pregnancy, postpartum period, menopause, adolescence. Climate change is also a physiological cause that does not require treatment. |
In addition to diseases, the cause of the development of orthostatic hypotension may be the intake of certain medications:
| Group of drugs | Examples of |
| Means that affect the tone of the nervous system. | Antipsychotic drugs, antidepressants, adrenergic blockers. |
| Sedatives | Barbiturates |
| Diuretic drugs. | Loop diuretics (furosemide, lasex). |
| Vasodilator drugs (vasodilators). | Nitrates, slow calcium channel blockers. |
| Drugs that affect the heart rate. | Antiarrhythmic drugs (quinidine, novocainamide). |
In addition, the intake of alcohol and drugs that contain ethyl alcohol has a strong effect on blood pressure.
Symptoms
Orthostatic hypotension manifests itself with a sharp rise from a horizontal position, it can also be with a long stay in a standing position.
Typically, the following symptoms are present:
- Headache of a pressing nature, localized in the occipital region.
- Dizziness.
- Great weakness.
- Darkening in the eyes.
- Noise in ears.
- Feeling of faintness, nausea.
- Cold sweat.
- Chills, cold extremities.
- Decrease in blood pressure.
With the development of an attack, a person feels the approach of fainting, this is the so-called pre-syncopal state. The senses are sharpened (hearing and sight). It may seem like time is slowing down. Fainting is possible. With a mild course, it is enough for a person to take a horizontal or sitting position to improve his health.
Sometimes the clinical picture can give an accurate idea of orthostatic hypotension. But in order to accurately diagnose the pathology and identify its cause, it is necessary to carry out additional diagnostics. To do this, you need to consult a neurologist, this specialist is engaged in the diagnosis and treatment of orthostatic hypotension.
He will order the following studies:
- Taking anamnesis and examining the patient. It is important to ask the patient if they are taking medications that can affect blood pressure.
- ECG.
- Daily Holter monitoring.
- TILT test (measurement of blood pressure when changing the position of the patient's body).
- Vagus tests (irritation of the vagus nerve).
- Ultrasound of the heart.
- General urine analysis.
- Clinical blood test.
- Blood chemistry.
- Blood test for hormones.
- Abdominal ultrasound.
First aid
First aid is aimed at preventing injury to the patient and the development of possible complications, including collapse.
The assistance includes the following measures:
- Lay the patient on his back, the head should be in an elevated state.
- Loosen the fasteners on the patient's clothes.
- Provide fresh air.
- If the patient is unconscious, then his head must be turned to one side in order to avoid aspiration of the respiratory tract with vomit (in case of a gag reflex).
- If a person is conscious, then you need to make him strong tea.
- If there is fainting (short-term loss of consciousness), ammonia will help bring you to your senses. It must be applied to a cotton swab and brought to the patient's respiratory tract, at a distance of about 15-20 cm.
- Measure blood pressure.
If a person, after applying these measures, remains unconscious or his condition worsens, it is necessary to call an ambulance.
Drug treatment
Orthostatic hypotension is a condition, the treatment of which must be comprehensive. Therapy includes not only taking medications, but also changing lifestyle and diet.
But drug treatment is a fundamental principle of therapy:
| Drugs | Mechanism of action | Examples of |
| Beta blockers | They have an effect on the adrenal cortex, retain sodium in the body, and increase vascular tone. | Propranolol |
| Mineralocorticoids | Increase vasospasm. | Florinef, Cortinef. |
| Adrenergic drugs (adrenomemetics) | Peripheral vessels are narrowed. | Droxidopa |
| Adaptogens | They stimulate the processes occurring in the central nervous system and the sympathetic division of the autonomic nervous system. | Eleutherococcus tincture |
| Vitamins of group B | They increase the resistance of the nervous system to various traumatic factors. | Milgamma (intramuscularly, deeply, 1 time per day) |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | Improves peripheral vascular resistance | Indomethacin (25-50 mg 3 times a day) |
Recommended diet
The principle of the diet for orthostatic hypotension is adequate salt intake. In case of hypotension, the recommended dose of consumed salt is 8-10 g per day. If there is an increase in blood pressure above 140 mm Hg. Art., then the amount of salt must be reduced to 6 g per day. Adequate intake of sodium in the body can be ensured by adding salt to food.
The active intake of salt into the body can provoke the development of edema, disturbances in the work of the myocardium and provoke acute heart failure. Therefore, during such a diet, it is necessary to control the level of blood pressure and body weight. And also it is necessary to regularly undergo an ECG and take a urine test to assess the state of the body.

With any changes, an increase in edema or irregularities in the work of the heart, the dosage of salt in the diet is reduced.
Otherwise, the patient must adhere to the foundations of a balanced diet. It is necessary to eat often, but in small portions, to avoid overeating and sudden weight gain. The diet should include fruits and vegetables, nuts and dried fruits.
It is better to limit the consumption of meat, but it should not be completely ruled out. Beef and pork can be eaten 3-4 times a week, the rest of the days it is better to give preference to lean meats (chicken, turkey), fish, seafood and plant foods.
Drinking regimen is another important part of maintaining balance for the patient with orthostatic hypotension. As with healthy people, the amount of fluid consumed should be at least 2 liters of fluid per day. You can drink still water, tea, juices and fruit drinks. It is better to replace green tea with black. If a person loves coffee, then with orthostatic hypotension, you can drink it.

The basic rule should be the choice of the drink: coffee from whole beans is preferable, not instant coffee. In addition to coffee, you can drink chicory, which has a beneficial effect on blood pressure levels.
Alcohol is excluded in patients with orthostatic hypotension.
In addition to the main fluid intake with orthostatic hypotension, an additional fluid intake is prescribed. The patient drinks 200 ml of liquid 6-8 times a day.
Complications and consequences
Orthostatic hypotension is a pathology with the development of which the following complications are possible:
- Fainting. It is characterized by short-term loss of consciousness.
- Collapse. It is a sharp drop in blood pressure and a violation of the blood supply to organs.
- Stroke. It can occur if the patient has pathological changes in the vessels of the brain. Sudden changes in blood pressure can affect the thinning of the walls of blood vessels, the formation of blood clots and ischemia (vasoconstriction).
- Injuries. Occur when a person falls. A fracture of the base of the skull is the most formidable complication of fainting.
- Diseases of the cardiovascular system. Constant drops in blood pressure reduce the contractile function of the myocardium and lead to the development of its functional insufficiency. As a result, the development of myocardial infarction, coronary heart disease and angina pectoris is possible.
- Disturbances in the work of the nervous system due to frequently repeated episodes of oxygen deprivation.
- Changes in the function of the organs of the urinary system (kidneys).
- Progression of chronic diseases of the central nervous system.

Collapse is a life-threatening condition that must be stopped urgently. This pathological condition often accompanies orthostatic hypotension. It is accompanied by weakness, dizziness, chills, cold sweats, decreased heart rate.
On examination, the patient is pale, facial features are sharpened, breathing is rapid, blood pressure is sharply reduced. The patient may be conscious, his reactions are inhibited, the reaction of the pupils is reduced.
The main difference between collapse and fainting is more pronounced vascular insufficiency, which can lead to the death of the patient. During fainting, compensatory mechanisms are preserved, which allows the patient to recover faster. Fainting does not carry any serious complications for life and health.

Fainting is the most common companion of orthostatic hypotension.
Represents a sharp loss of consciousness against the background of short-term hypoxia (lack of oxygen) of the brain:
- Tinnitus.
- Darkening before the eyes.
- Cold sweat.
- Feeling sick.
- Nausea.
- Yawn.
- Sharp weakness, feeling of "cottony" legs.
The attack lasts from two to 30 minutes. In severe cases, involuntary urination is possible.
The prognosis for orthostatic hypotension is favorable. By following the prescribed treatment and preventing recurrent attacks, possible complications can be minimized. To do this, it is necessary to strictly observe the dosage of the prescribed drugs, adhere to a diet and drinking regimen, and observe a mode of work and rest.
In addition, do not forget about the correct rise from a horizontal position, it should be slow and smooth. This is especially true for the elderly and pregnant women.
Disease video
Living healthy: orthostatic hypotension: