Blood flow supplies the cells of the human body oxygen and nutrients. It consists of the heart and blood vessels that run through the body. The vascular scheme resembles a tree: thick arterial branches branch off from the "trunk", the main artery, and branch out further and further. The smallest arteries end in a network of tiny blood vessels called a capillary network.
Record content:
-
1 Characteristic
- 1.1 How veins are subdivided
- 2 Functions and properties
-
3 Anatomy and structure
- 3.1 Arterial wall structure
- 3.2 Arterioles
- 3.3 Capillaries
- 3.4 Venules
- 3.5 Veins
-
4 Possible diseases and pathologies
-
4.1 Atherosclerosis
- 4.1.1 Classification
- 4.1.2 Symptoms and Signs
- 4.1.3 Causes
- 4.1.4 Treatment methods
-
4.2 Peripheral artery disease
- 4.2.1 Classification
- 4.2.2 Symptoms and Signs
- 4.2.3 Causes
- 4.2.4 Treatment methods
-
4.3 Vasculitis
- 4.3.1 Classification
- 4.3.2 Symptoms and Signs
- 4.3.3 Causes
- 4.3.4 Treatment methods
-
4.1 Atherosclerosis
- 5 Video about the human circulatory system
Characteristic
Human blood vessels, the circuit of which is a closed system of tubes, transport blood to all organs and back to the heart. Structurally and functionally, all vessels are interconnected, like any biological system.
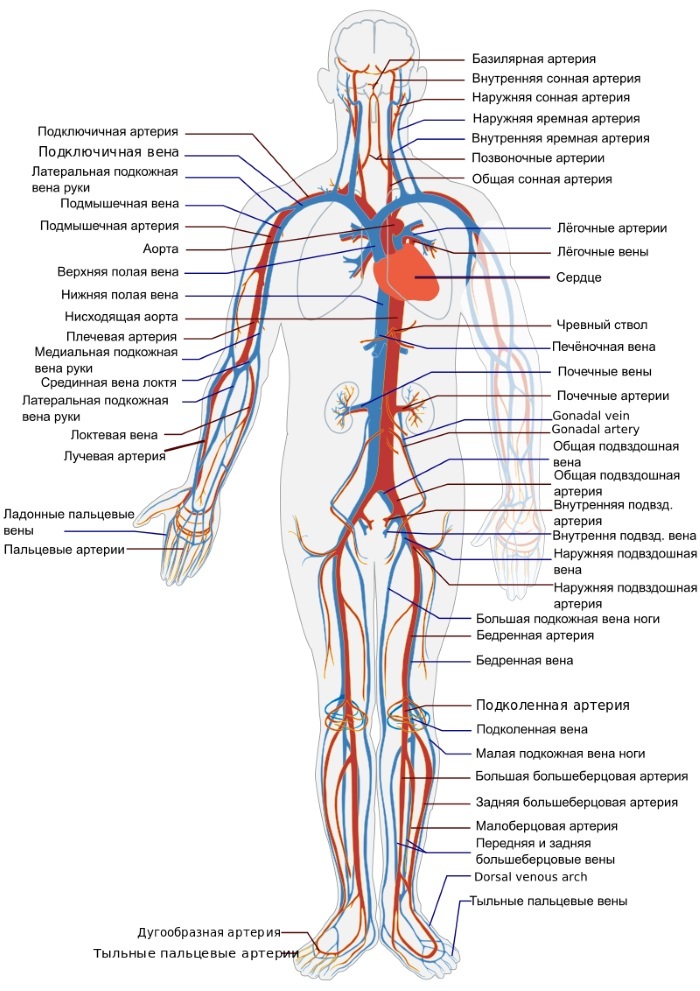
Various types of vessels are involved in the process of systemic blood flow:
- aorta (artery);
- arteriole;
- capillary;
- vein;
- venula;
- coronary vessels.
First, blood is pumped from the left heart ventricle into a large artery called the aorta. The aortic vessel branches into large arteries that supply blood to cells in both the upper and lower body. The major arteries continue to branch out into smaller arteries called arterioles. Numerous branching arterioles then pass into the capillaries.
Blood is transported in 2 different ways: through the systemic and pulmonary circulation.
The systemic arteries provide oxygen to tissues and organs and are branches of the aorta. The aorta rises from the left ventricle, curves posteriorly and to the left, then descends through the chest and abdomen. On its way, it divides into 3 parts: the ascending aorta, the arch and the descending aorta. The descending one consists of the thoracic and abdominal aorta.
How veins are subdivided
- The deep ones pass in the muscle tissue. Superficial veins are located closer to the surface of the skin
- The pulmonary veins carry oxygenated blood to the heart. Each lung has a right and left vein.
Systemic veins are located throughout the body from the legs to the neck. They transport deoxygenated blood back to the heart. There is a separate part of the blood flow system, the coronary circulation, which is responsible for providing the heart with a constant flow of blood.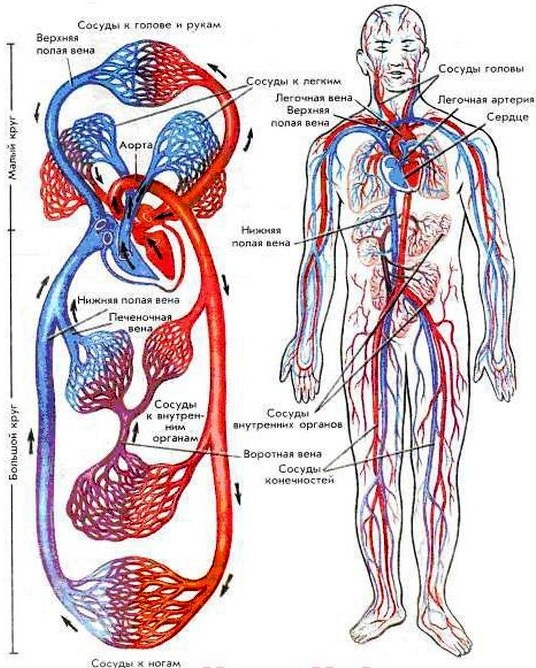
Coronary circulation, if you look at the atlas of blood vessels, is depicted as a small loop in the systemic circulation, through which blood is carried only from the heart and back to the heart. The two main coronary arteries are located here - the left and right coronary arteries.
Functions and properties
Human blood vessels (the branching diagram is presented on the website) ensure the survival of the organism. Blood, as a vehicle, supplies organs primarily with oxygen. It also delivers nutrients and hormones.
The key function of the vascular system: intake, transport and use of oxygen during physical activity, resting state. The disturbed rhythm of blood flow in the heart and lungs often has serious consequences for a person.
Anatomy and structure
The arteries transport blood to the tissues of the body under high pressure, which is created by the pumping action of the heart. The heart pumps blood into these elastic tubes, which send blood in pulsating waves.
Therefore, it is imperative that the vessels have strong elastic walls to ensure rapid and efficient blood flow to the tissues.
Arterial wall structure
| Name | Characteristic |
| Intimate tunic (inner layer) | Consists of smooth endothelium, which is poured into the surface of the inner elastic tissue. |
| Tunic media (middle layer) | The middle shell, the thickest, consists of smooth muscle cells mixed with elastic fibers. In larger vessels, the middle membrane consists mainly of elastic fibers. As the arteries get smaller, the number of elastic fibers decreases and the number of smooth muscle fibers increases. |
| Adventitia tunic (outer layer) | This layer is the most durable of the 3 layers. It is composed of collagen and elastic fibers. The adventitia membrane provides a restraining barrier that protects the vessel from over-expansion. Characteristic of this layer is the presence of small blood vessels called vasa vasorum (vascular vessels) that supply blood walls of larger arteries and veins, while the inner and middle layers of blood vessels are nourished by diffusion of blood as it transportation. The thicker and more elastic wall of the arteries allows them to expand with the pulse and return to their original size. |

The arteries near the heart have the thickest walls, containing a high percentage of elastic fibers in all 3 membranes. These are elastic or conductive arteries.
Arterioles
Arteries become arterioles. The transition occurs gradually, with a progressive thinning of the vessel wall and a decrease in the size of the lumen or passage.
In arterioles, the inner sheath is present in the form of a lining covered with a layer of thin longitudinal fibers, but the middle the shell no longer contains elastic fibers and consists of only one layer of round or spiral smooth muscle fibers. The adventitia consists of connective tissue elements.
Capillaries
Small arteries and arterioles act as control valves through which blood enters the capillaries. Their function is to resist and regulate blood pressure.
As the arterioles decrease, the 3 membranes become less and less defined. The smallest arterioles are composed of almost a single endothelium and are surrounded by a layer of smooth muscle. Microscopic capillary tubules consist of a single layer of endothelium, which is an extension of the inner lining cells of arteries and veins.
Capillaries are the smallest and most numerous blood vessels in the systemic circulation. They form a branched mesh structure known as a capillary bed, found in all structures of the body.
Venules
When the capillaries converge, they form venules, whose function is to collect blood from the capillary beds (capillary networks). Venules consist of an endothelial tube supported by a small amount of collagen tissue, while larger venules have several smooth muscle fibers.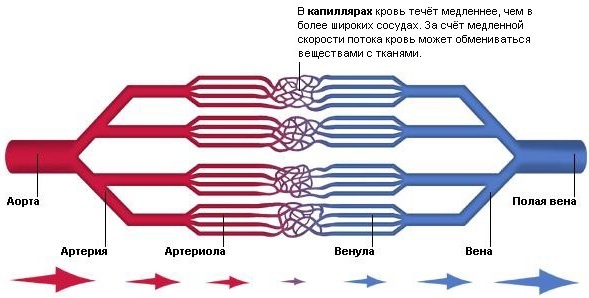
As the venules continue to grow in size, the walls of the vessels acquire the structure characteristic of arteries, although they become much thinner. These small vessels also have a protective effect: in those places where the infection has developed, the venules secrete leukocytes to fight foreign cells.
Veins
The veins that function to carry blood from peripheral tissues to the heart have endothelial a lining surrounded by a membrane that contains less muscle and elastic tissue than the wall arteries. The outer layer, tunica adventitia, consists mainly of connective tissue.
Since the blood pressure in these vessels is extremely low compared to the arterial system, and blood must come out when even lower pressure, then this creates the need for a special mechanism for the further advancement of blood and its return to a heart. For the forced movement of blood, many vessels have a unique valve system.
The valves, formed by the semilunar folds in the inner lining, are arranged in pairs and serve to direct the flow of blood to the heart, especially in an upward direction.
When blood flows to the heart, the valve flaps rest against the vein wall, and then they block the opening when the pressure of blood and surrounding tissue fills the valve pocket. There are many more of these valves in the veins of the extremities than in other parts of the body.
Veins are more extensible than arteries, and their walls are designed to allow them to expand or contract. The main function of their contractility is to reduce the capacity of the cardiovascular system due to constriction of peripheral vessels in response to the heart's inability to pump enough blood.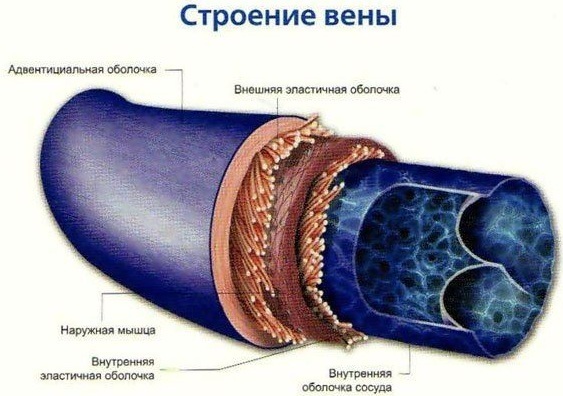
Veins, as a rule, run parallel to the arteries, but are present in greater numbers. Their canals are larger, arterial, and their walls are thinner. About 60% of the blood volume is in the systemic circulation, and 40% is concentrated in the veins.
Possible diseases and pathologies
Despite the presence of valves, and other anatomical and physiological devices of blood flow, during day, some blood will inevitably accumulate, especially in the lower limbs, due to strength severity.
The blood that collects in a vein increases pressure inside it, which can then be reflected back into smaller veins, venules, and eventually capillaries, causing them to bloat.
Human blood vessels (the diagram of their relationship with organs is well represented in the medical atlas) are also susceptible to various diseases. It is associated with enlargement, narrowing, or hardening of the arteries and veins.
Atherosclerosis
Atherosclerosis, a chronic disease caused by the deposition of fats, cholesterol, calcium and other substances in the innermost layer of large and medium arteries.
Atherosclerotic accumulation is often found in the aorta and large aortic branches. Coronary artery disease, which decreases blood flow to the heart muscle, leads to coronary artery disease, a chest pain known as angina.
Classification
Atherosclerosis has various forms, depending on the affected vessels. Distinguish between microangiopathy, affecting large and medium arteries, and microangiopathy, which develops in arterioles, capillaries or venules. The latter disease usually occurs in diabetes mellitus.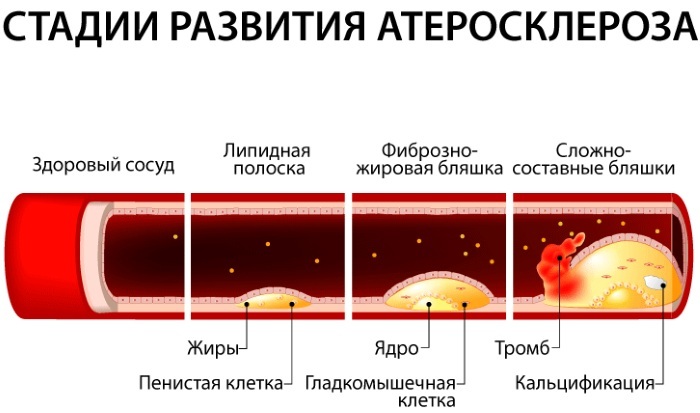
Forms of atherosclerosis:
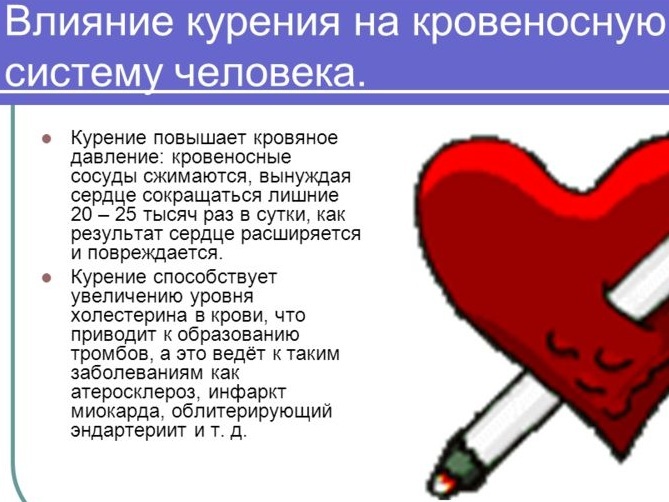
- Minor, in which the endothelium is damaged. Provoking factors: high blood pressure, smoking.
- Moderate. The damage triggers an inflammatory response and leukocytes deposit cholesterol to form atheroma. Calcium salts and fibrous tissue form deposits on the walls of blood vessels. The artery loses its elasticity and narrows.
- Heavy. Deposits on the walls of blood vessels restrict blood flow. High blood pressure contributes to the formation of a large number of plaques.
Symptoms and Signs
Atherosclerosis can go on for years without any symptoms. Common manifestations include coronary artery disease, infrarenal aortic aneurysm, cerebrovascular disease, and peripheral arterial disease.
Causes
The exact mechanisms of atherosclerosis are not fully understood, but in some people, the disease can begin in childhood with the formation of tiny "fat streaks" or streaks of fat deposits in the arteries.
First order risk factors:
- Nicotine abuse: Smoking contributes to the early onset and rapid progression of atherosclerosis.
- Arterial hypertension: Due to increased pressures, damage to the endothelium occurs faster. Arterial hypertension is the main risk factor for the development of cerebrovascular insufficiency.
- Diabetes mellitus: Increased phagocytosis and endothelial damage are the result of reactive glycosylation due to elevated blood glucose levels.
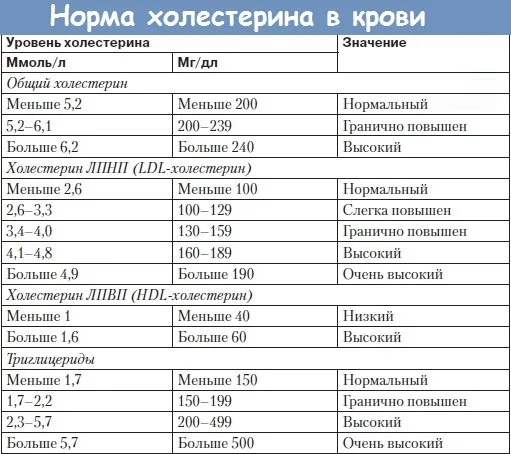
- Hyperlipoproteinemia: Excess LDL cholesterol increases the risk of atherosclerosis, especially when combined with low HDL cholesterol.
The reasons why the development of atherosclerosis leads to form 2 are as follows:
- lack of exercise;
- stress;
- obesity;
- increased content of uric acid in the blood;
- excess triglycerides in the blood, which often gives rise to the development of acute pancreatitis;
- increased levels of fibrinogen in the blood;
- accumulation of homocysteine (sulfur-containing amino acid) in the blood;
- impaired glucose tolerance;
- chronic renal failure;
- elevated lipoprotein levels.
Treatment methods
Many medicines can reduce the risks associated with atherosclerosis. These include statins, which lower cholesterol and blood fat, as well as anticoagulants and other drugs such as aspirin, which prevent blood clots.
In large arteries, such as the aorta or carotid artery, areas blocked by atheromas can be surgically removed and replaced with synthetic materials.
Atherosclerotic plaques can also be removed from the carotid artery circulation using atherectomy.
The vessels of the coronary arteries in case of occlusions restore blood flow after coronary artery bypass grafting. The scheme of the operation is that sections of blood vessels from other parts of the human body are used to redirect blood flow around obstacles. Balloon angioplasty is often used.
Peripheral artery disease
Peripheral artery disease, often called PAD for short, is a narrowing of the blood vessels that carry oxygenated blood to the peripheral regions of the body.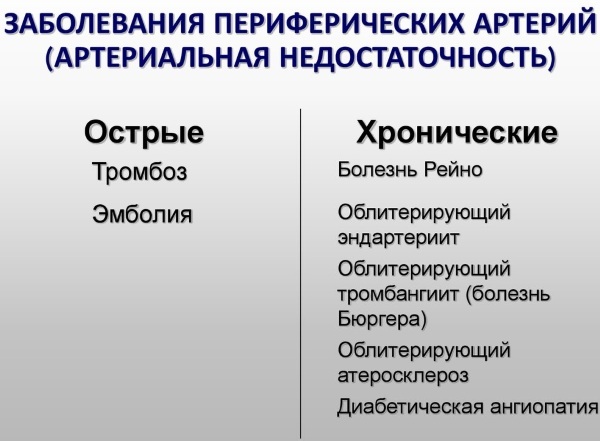 This condition affects the arteries in the legs or pelvis.
This condition affects the arteries in the legs or pelvis.
Classification
For this disease, a classification has been developed:
- 0 degree: the lesion proceeds without ulcers, without gangrene.
- Grade 1: There is a shallow, shallow ulcer, but no gangrene.
- Grade 2: A deep ulcer develops with an exposed tendon or bone, and gangrene is limited to the toes.
- Grade 3: Large, full-thickness ulcer, gangrene extending to the forefoot or midfoot.
Symptoms and Signs
Human blood vessels (the peripheral artery pattern includes the abdominal aorta, the arteries of the lower extremities and the pelvis) are narrowed due to the formation of atherosclerotic plaques. PAD almost always goes unnoticed or is mistaken for another condition.
This is because symptoms include cramping, pain, heaviness in the legs or thigh muscles, which disappear when the person rests. In the future, a person begins to notice constant pain in the legs and hips, wounds that appear in these areas that do not heal properly and seem cold to the touch.
Causes
Like other heart diseases, it is caused by the accumulation of fat, cholesterol, and calcium on the inner walls of blood vessels.
Risk factors:
- Smoking.
- High blood sugar.
- High cholesterol.
- Increased blood pressure.
- Other risk factors, which include levels of various inflammatory mediators such as C-reactive protein, fibrinogen, homocysteine, and lipoprotein A.
Treatment methods
Medical treatment includes:
- Diabetes management.
- Hypertension management.
- Reducing high cholesterol levels.
- Antiplatelet drugs such as aspirin and clopidogrel.
Statins reduce clot formation and cholesterol levels, respectively, may help stop progression of the disease and eliminate other cardiovascular risks that arise in victim.
Vasculitis
Human blood vessels, which are profusely bifurcated, often become inflamed, causing wall changes, including thickening, weakening, narrowing, or scarring. Systemic diseases, in which the walls become inflamed, restrict blood flow, resulting in damage to other organs and tissues.
Classification
There are many types of vasculitis and most are rare. The disease affects one or more organs. The condition can be short-term (acute) or long-term (chronic).
Vasculitis is also known as angiitis and arteritis.
- Behcet's disease. This condition causes inflammation of the arteries and veins. Signs and symptoms include mouth and genital ulcers, eye inflammation, and acne-like skin lesions.
- Burger's disease. It is characterized by inflammation and blood clots in the blood vessels of the arms and legs, resulting in pain and ulcers in these areas. Rarely, blood vessels in the abdomen, brain, and heart are affected.
- Giant cell arteritis. The disease is accompanied by inflammation of the arteries of the head, especially the temples. Giant cell arteritis can cause headaches, scalp soreness, jaw pain, blurred or double vision, and even blindness. It is also called temporal arteritis.
-
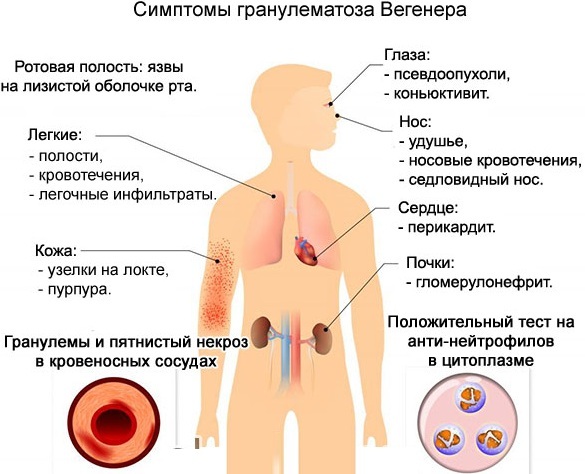
Wegener's granulomatosis. The disorder causes inflammation of the blood vessels in the nose, sinuses, throat, lungs, and kidneys. Signs and symptoms include nasal congestion, sinus infections, nosebleeds, and possibly a bloody cough
- Purpura Genoch-Schönlein (IgA vasculitis). This condition is more common in children than in adults and causes inflammation of the tiny blood vessels (capillaries) of the skin, joints, intestines, and kidneys. Signs and symptoms include abdominal pain, blood in the urine, joint pain, and a rash on the buttocks or lower legs.
- Microscopic polyangiitis. This form of vasculitis affects small blood vessels, usually in the kidneys, lungs, or nerves. Abdominal pain and rash, fever, muscle pain and weight loss may appear.
- Takayasu's arteritis. This form affects the larger arteries in the body, including the aorta. Signs and symptoms include joint pain, loss of pulse, high blood pressure, night sweats, fever, general malaise, loss of appetite, headaches, and visual changes.
Symptoms and Signs
Common signs of vasculitis include:
- high fever;
- headache;
- increased fatigue;
- weight loss;
- pain in many parts of the body;
- night sweats;
- rash;
- nerve problems such as numbness or muscle weakness.
Causes
The exact cause of vasculitis is not fully understood. Some types are associated with a person's genorm. Others arise when the immune system mistakenly attacks the cells of the blood vessels.
Possible triggers for this immune system response include:
- Infections such as hepatitis B and hepatitis C.
- Blood cancer.
- Diseases of the immune system such as rheumatoid arthritis, lupus and scleroderma.
- Reactions to certain medications
Treatment methods
Treatment focuses on controlling inflammation with medication and eliminating any underlying disease that caused it. A 2-phase treatment is carried out - first, inflammation is stopped, and then relapse is prevented (supportive therapy). Both phases involve prescription drugs.
The doctor may prescribe:
- corticosteroid medications such as prednisone or medrol to control inflammation;
- steroid-sparing: Methotrexate, Azathioprine, Mycophenolate or Cyclophosphamide.
The exact medication you will need depends on the type and severity of the vasculitis, the organs involved, and any other medical problem. Depending on the type of disease, biological treatment methods, such as Rituxan or Actemra, may be recommended.
Sometimes, with vasculitis, a balloon bulge (aneurysm) forms in the blood vessel wall, which may require surgery. If the arteries are blocked, surgery is also done.
As a rule, the operation is not suitable for diseases of the blood vessels, since the vessels are difficult to operate because they are irreversibly damaged. However, there are a number of medications that are used in medical conditions to prevent the narrowing of the blood vessels.
Common medications include:
-
Nitroglycerine, which can be used to dilate arteries and improve blood flow.

The effect of nitroglycerin on the body - Ranolazine - helps to alter sodium and calcium levels to relieve common chest pain.
- Beta blockers - designed to slow down the heart rate, which in turn lowers blood pressure.
- Calcium channel blockers - designed to help relax the muscles around the coronary arteries, improve blood flow, and reduce the chance of blockages.
- Statins are designed to lower cholesterol, which also helps to increase blood flow.
- Aspirin Is a very common medicine that is prescribed to people to limit inflammation and prevent blood clots. However, aspirin should not be used in people already on blood thinning medications, medications for other heart conditions, as it can cause additional health problems.
Healthy blood flow is critical to human health. Physical activity is one of the best ways to achieve and maintain optimal heart and lung function.
If you have health problems, you should consult your doctor to find out which scheme adhere to better preservation of the frequency and rhythm of the pulse, and therefore, the efficiency of the blood vessels. This is one of the most important things that will ensure a long and fulfilling life.
Video about the human circulatory system
Blood vessels:


