1 Clinical picture of the pathology of
Pancreatitis is an acute or chronic inflammatory disease of the pancreas of various etiologies. As it proceeds, not everyone knows. Often this pathology leads to destruction and necrosis. Pancreatitis is a group of diseases united by a common clinical picture and pathogenesis. Acute inflammation of the pancreas is the third most common among all diseases of the abdominal cavity.
Do you have pancreatitis?
Natalia Ronina: "How did I manage to beat pancreatitis at home for 1 week, paying 30 minutes a day? !" Read more & gt; & gt;
Every year about half a million cases of this disease are diagnosed. Among the patients, males predominate. This is due to a great predilection for alcohol and fatty foods. Of all the diseases, pancreatitis is different in that it often develops in young people who abuse alcohol.
The peak incidence falls on the age of 30 to 40 years. Often, this pathology is combined with cholelithiasis. In this case, the main contingent of patients will be elderly people over 60 years old.
2 Types of
Do not just know what pancreatitis is, but also have an idea of its varieties. By the nature of the flow, the following forms of pancreatitis are distinguished:
- acute;
- acute recurrent;
- chronic;
- chronic during an exacerbation.
The difference of the chronic form is that it undergoes destruction( destruction) of the organ. Very often acute pancreatitis becomes chronic. The latter can disturb a person for more than one year. About recurrent acute inflammation it comes when the pancreatic syndrome occurs in the first six months of the onset of the disease. There are also pancreatonecrosis and edematous form of the disease. In the first case, the process of cell death starts.

Recommended to read
- Menu for pancreatic pancreatitis
- Causes of diffuse pancreatic changes
- Symptoms of pancreatitis in children
- Effective agent for gastritis and gastric ulcer
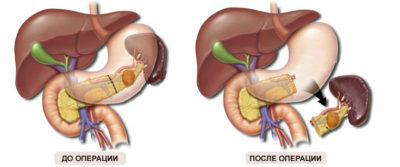
Foci of necrosis are formed. They are small, medium and large. In very severe cases, total necrosis of the gland is observed. In this situation, it may be necessary to remove the organ. With edematic form, necrosis areas are not formed. This form of the disease is characterized only by an increase in the gland in the volume and a violation of its function.
3 What is acute pancreatic inflammation?
The causes of pancreatitis( pancreatic disease) are varied. The most important factors are the following predisposing factors:
- bile flow disorder;
- alcohol abuse;
- acute poisoning;
- excess in the diet of fatty foods;
- presence of cholelithiasis;
- abdominal trauma;
- diabetes;
- helminthiases and other parasitic diseases;
- cirrhosis;
- treatment with glucocorticosteroids, antibiotics and hormonal drugs;
- vascular disorders;
- narrowing or inflammation of the sphincter of Oddi;
- of duodenal disease( ulcer or duodenitis);
- cystic fibrosis;
- Vascular pathology( vasculitis);
- viral and bacterial diseases;
- congenital malformations;
- introduction of the vaccine.
-
 IMPORTANT TO KNOW! Gastritis? Ulcer? To have a stomach ulcer not turned into cancer, drink a glass. ..Read the article & gt; & gt;
IMPORTANT TO KNOW! Gastritis? Ulcer? To have a stomach ulcer not turned into cancer, drink a glass. ..Read the article & gt; & gt;
In women, inflammation of the pancreas often develops against a background of cholelithiasis. In children, cystic fibrosis is a common cause. The most common causes of pancreatitis are alcoholism and malnutrition. Alcoholic pancreatic damage is more common among young men after the age of 35 years. Chronic pancreatitis develops if a person consumes more than 20 ml of alcohol daily for 5-20 years.

Exacerbates the situation of excess protein and fatty foods in the diet. Negatively affects the condition of the body smoking. Cigarette smoke contains a lot of toxic substances that increase the secretion of the gland. The pancreatic juice begins to digest the organ, causing swelling. The disease can occur in individuals whose parents have suffered from this pathology.
-
 Gastroenterologist. IMPORTANT: "I beg you, if you started to worry about abdominal pain, heartburn, nausea, do not do gas in any way. .."Read more & gt; & gt;
Gastroenterologist. IMPORTANT: "I beg you, if you started to worry about abdominal pain, heartburn, nausea, do not do gas in any way. .."Read more & gt; & gt;
4 Symptoms of acute form
The most common acute form of the disease. At the heart of its development are the following processes:
- disruption of pancreatic juice production;
- enzymatic autoaggression( irritation of the mucous organ with its own enzymes);
- cell death.
A secondary bacterial infection is often attached. With the development of acute pancreatitis, the following symptoms are present:
- pain in the epigastric zone or hypochondrium on the left;
- fever;
- nausea;
- vomiting;
- of jaundice;
- change in blood pressure( hypertension or hypotension);
- hiccups;
- change of complexion;
- stool disorder by type of diarrhea or constipation;
- bloating( flatulence);
- cyanotic skin tone;
- burp;
- dry mouth.

Acute pancreatitis is always painful. It arises suddenly against a background of good health. Often it appears at night. Such patients wake up and can not fall asleep. Pain has the following features:
- intense;
- constant;
- sharp;
- piercing;
- is felt in the epigastric zone or in the left hypochondrium;
- is combined with vomiting and nausea;
- radiates into the back;
- is prone to gain;
- is sometimes shrouded.
Pain does not allow a person to engage in daily activities. Such people rush about the room, can not find a place. Often patients take a forced position of the body( with knees bent at the knees or on all fours).Pain in pancreatitis is not like colic. An attack can occur after drinking alcohol, spicy or fatty foods.
ADVICE FROM THE MAIN GASTROENTEROLOGIST
Korotov SV: "I can recommend only one remedy for the rapid treatment of Ulcer and Gastritis, which is now recommended by the Ministry of Health. .." Read testimonials & gt; & gt;
Many patients change appearance: the skin first becomes pale, but then acquires a grayish hue. There is a sharpening of facial features. Sometimes, around the navel or in the lumbar region, small blue spots appear. Acute inflammation often occurs with severe fever.
Vomiting is a single or multiple. After it, a person does not get better. Vomit contains bile. A typical manifestation of acute pancreatitis is a change in stool. It becomes mushy, liquid and foamy.

It contains undigested food residues. The chair has a sour, fetid smell. Some patients have constipation. The abdomen becomes firm. The sclerosing form of the disease is often manifested by jaundice.
5 Symptoms of chronic pathology
Two periods are distinguished in the development of chronic pancreatitis: initial and destructive changes. The first - lasts about 10 years. In this phase, patients complain of pain. It is felt at the top of the abdomen, in the region of the heart, left side or in the waist. It can mimic angina and renal colic. With total organ damage, pain is shrouded.
WE RECOMMEND!
For prophylaxis and treatment of Digestive Gastrointestinal Diseases our readers advise Monastic tea. This unique remedy consists of 9 medicinal herbs useful for digestion, which not only supplement, but also strengthen each other's actions. Monastic tea will not only eliminate all symptoms of the gastrointestinal tract and digestive system, but will also permanently eliminate the cause of its occurrence.
Opinion of doctors. .. "
Pain syndrome decreases when a person sits. Discomfort appears 15-20 minutes after eating. Pain syndrome in chronic pancreatitis is combined with dyspeptic disorders. The external secretory function does not suffer. When the disease progresses, morphological changes in the tissue are observed. Enzymatic insufficiency develops.

Its appearance is due to cell death and atrophy of glands. During this period, dyspeptic disturbances come to the fore in the clinical picture. Chronic inflammation of the gland manifests itself as a violation of the digestive process. Due to maldigestia and malabsorption( violation of the decomposition of food and its absorption), the character of the chair changes.
Stool analysis is of great diagnostic value. The feces become crusty, fat with a sour smell. Dyspepsia leads to increased formation of gases in the intestines, which causes bloating. Patients lose weight. Chronic pancreatitis is characterized by symptoms of hypovitaminosis. Lack of vitamin A leads to a violation of skin pigmentation.
Hypovitaminosis of vitamin C and K is manifested by bleeding gums, brittle nails, hair loss. The lack of cyanocobalamin and folic acid causes anemia. At a pancreatitis calcium exchange is quite often broken. Calcium is poorly absorbed, which leads to brittle bones( osteoporosis).The lack of calcium is manifested by a convulsive syndrome.
Some patients in the abdomen and chest appear reddish spots. Other possible manifestations of chronic pancreatitis include dry skin, presence in the language of white plaque, jaundice, tenderness of the abdomen during palpation, a slight increase in the liver and spleen. Against the background of this disease often develops diabetes.

6 Possible complications of
Acute form of inflammation can lead to the following consequences:
- bleeding;
- ascites( accumulation of fluid in the abdominal cavity);
- pain shock;
- loss of consciousness;
- reduced diuresis;
- skin rash;
- encephalopathy;
- psychosis;
- blood clotting disorder;
- heart damage( myocarditis);
- multiple organ failure;
- formation of abscesses;
- education pseudo-caster.
Despite the fact that chronic pancreatitis is not as bright as acute, it can also lead to formidable complications. Against the background of chronic inflammation of the gland can develop diabetes, thrombosis, narrowing the gatekeeper. The most dangerous complication is the formation of adenocarcinoma. This is a malignant tumor. Most often, it is formed with a prolonged course of the disease( more than 20 years).
7 Types of therapy
You need to know not only what pancreatitis is, but also how to treat it. If symptoms of inflammation of the gland appear, the patient should be assisted and examined. Diagnosis includes ultrasound of the abdominal cavity organs, analysis of feces, blood and urine, physical examination, magnetic resonance imaging, FGDS.Acute pancreatitis in the absence of complications passes independently.

When an attack of acute pancreatitis develops, the patient should be placed in a semi-sitting position with his legs pressed, and also make sure that he does not take food. Fasting for 2-3 days has a therapeutic effect. Every 2 hours you need to drink a glass of clean water. With acute pain, you can put ice under your back.
Enzyme drugs and pain medication are not accepted. After the diagnosis, medications for pain relief( NSAIDs or antispasmodics) are shown. In severe cases, parenteral nutrition is prescribed. From the stomach remove food and prescribe antacid preparations. The treatment regimen includes proteolysis inhibitors. The drug Octreotide is often used.
Infusion therapy may be required. Antibiotics are indicated to prevent infectious complications. In the case of necrosis, abscesses, the formation of cysts and stones, surgery is required. Patients should always follow a diet, give up alcohol and quit smoking.

8 Treatment of the disease
For the normalization of digestion in the case of development of secretory deficiency in the background of chronic pancreatitis, substitution drugs( Pansinorm, Mezim forte, Pancitrat) are shown.
Pancreatin is a disease that is treated very often. It is often appointed antatsidy and blockers H2-histamine receptors. For relief of pain, spasmolytics( Sparex, No-shpa, Drotaverin, etc.) are used.
In case of development of alcoholic pancreatitis it is necessary to refuse alcohol. If the enzyme drugs are ineffective, NSAIDs( Nimesulide, Diclofenac, Ibuprofen, Celecoxib) or analgesics are prescribed. With loss of body weight, triglycerides and complex vitamins are used. In the presence of purulent complications, surgical treatment is required.
In the phase of remission patients are recommended to drink mineral water and observe a strict diet. Diet No. 5B is prescribed. Not everyone knows how useful it is for the patient. It is required to avoid fatty foods, pickles, marinades, spices. In the presence of complications, patients should be treated in the hospital. Thus, pancreatitis is a dangerous disease, which is mainly caused by an incorrect way of life( inappropriate nutrition and alcoholism).
- 1 Clinical picture of pathology
- 2 Types of the disease
- 3 What is acute inflammation of the pancreas?
- 4 Symptoms of acute form
- 5 Symptoms of chronic pathology
- 6 Possible complications
- 7 Types of therapy
- 8 Treatment of ailment
Experienced doctors know what pancreatitis is dangerous, what kind of illness it is and why it appears. With an acute form of inflammation of the pancreas, one often has to deal with specialists in the surgical profile. This disease is fraught with formidable complications up to complete necrosis of the organ and the development of peritonitis.