Antiphospholipid antibodies are a group immune protein compounds (antibodies) that the body mistakenly produces against itself in an autoimmune-type response to phospholipids. Tests help detect autoantibodies that bind to phospholipids and increase the risk of excessive blood clotting.
Record content:
- 1 How and under what conditions are they produced?
- 2 API classifications
-
3 The reasons for the appearance of the increase
- 3.1 Symptoms of appearance and increase
- 3.2 Indications for research
-
4 How is it determined?
- 4.1 Preparation and analysis
- 4.2 Decoding the results
- 5 When to see a doctor
- 6 How to bounce back
- 7 Possible complications
- 8 APS video
How and under what conditions are they produced?
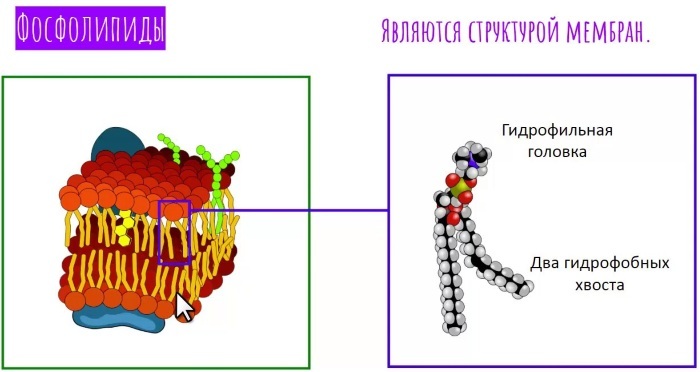
Phospholipids are structural components of tissue cells and play an important role in blood clotting. Phospholipids are critical for platelet function in addition to various coagulation cofactors.
When antiphospholipid antibodies are produced, they interfere with the clotting process. They increase the risk of developing recurrent inappropriate blood clots (blood clots). This can lead to strokes, heart attacks and / or miscarriages.
Antiphospholipid antibodies are associated with a low platelet count (thrombocytopenia) and the risk of recurrent miscarriages (especially in the 2nd and 3rd trimester), premature birth, and preeclampsia.
One or more antiphospholipid antibodies have been identified under various conditions:
- autoimmune disorders;
- lupus;
- rheumatoid arthritis;
- systemic sclerosis;
- infections;
- HIV;
- Mononucleosis;
- rubella;
- cancer cells.
Antiphospholipid antibodies, which can be tested by a family doctor, can cause antiphospholipid syndrome (APS), also called Hughes syndrome.
It is a recognized group of symptoms that includes blood clots, miscarriage pregnancy, platelet deficiency (thrombocytopenia), and the presence of one or more antiphospholipid antibodies. APS can be primary without an underlying autoimmune disorder, or secondary, existing with a diagnosed autoimmune disorder.
International Congress on Antiphospholipid Antibody Task Force Criteria for APS Detection Requires Cardiolipin Antibody Testing, anticoagulant lupus and antibodies to beta-2 glycoprotein in the presence of 1 of 2 clinical problems, blood clots (thrombosis), or morbidity during pregnancy.
The presence of an antiphospholipid antibody, such as anticoagulant lupus and anti-cardiolipin antibody, in an individual is associated with a predisposition to blood clots.
Blood clots can form anywhere in the body and lead to stroke, gangrene, heart attack, and other serious complications. In people with lupus, the risk of blood clotting does not necessarily correlate with disease activity, so the presence of these antibodies can cause problems even if lupus is under control.
Complications of antiphospholipid antibodies in lupus include:
- loss of a fetus or miscarriage;
- blood clots in veins or arteries (thrombosis);
- low platelet count (autoimmune thrombocytopenia);
- strokes that turn into ischemic attacks (stroke prevention);
- Liebman-Sachs endocarditis (formation of a clot on a specific heart valve);
- pulmonary embolism.
Many people with antiphospholipid antibodies have a purple or reddish lace pattern under their skin known as livedo. This pattern is especially noticeable on the limbs (i.e. arms and legs).
However, it is important to understand that having a livedo does not necessarily mean that a person has antiphospholipid antibodies.; rather, physicians recognize the correlation between the two conditions. Livedo may be associated with other blood vessel disorders.
API classifications
The false positive syphilis test was the first recognized test for antiphospholipid antibodies. In the 1940s, when people underwent “premarital check-ups,” doctors realized that some women with lupus might have positive results.
The Wasserman test depended on antibodies found in syphilis patients called reagin. The substance that this antibody reacts to is cardiolipin, so people with a false positive syphilis test actually had a form of antibodies against cardiolipin.
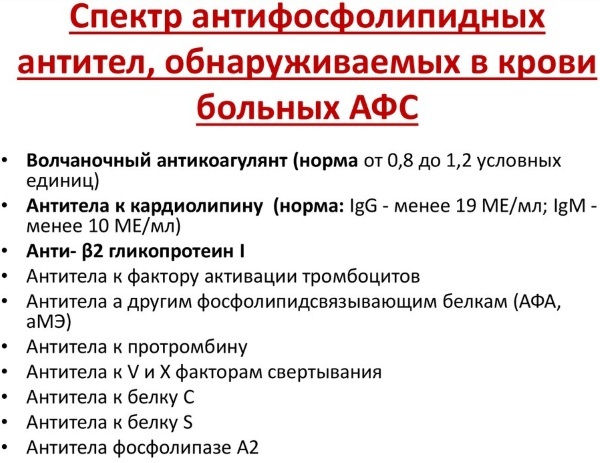
Tests called coagulation tests are used to detect the anticoagulant lupus (LA). Although the lupus anticoagulant causes blood to clot more easily in vivo (i.e. the human body), they actually cause a long time of blood clotting in vitro (that is, in test tube). Therefore, if it takes longer than usual for blood to clot.
Activated partial thromboplastin time (APTT) is often used to test for LA. If this test is negative, more sensitive tests for coagulation, platelet neutralization procedure (PNP) and kaolin clotting time (KCT) are performed. Usually, 2 of these tests (APT and RVVT) are performed to detect if a lupus anticoagulant is present.
Based on the foundations and testing, different classes (isotypes) of anticardiolipin antibodies were derived, namely:
- IgG;
- IgM;
- IgA.
IgG is the type of anti-cardiolipin antibody most commonly associated with complications. An enzyme linked immunosorbent assay (ELISA) is used to test for antibodies against cardiolipin. All isotypes can be tested at the same time or detected separately.
High levels of the IgM isotype are associated with autoimmune hemolytic anemia, a condition in which a person's immune system attacks their red blood cells.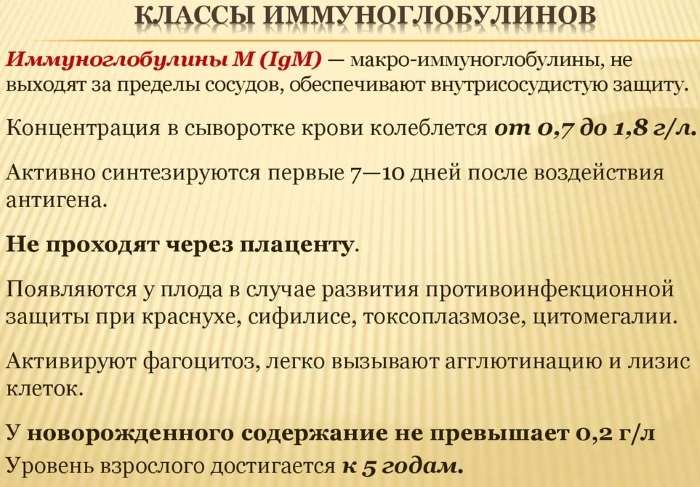
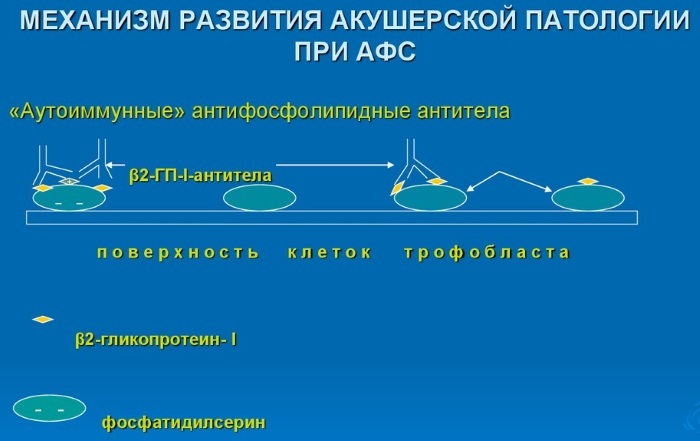
Anti-beta2 glycoprotein 1 - Beta2 glycoprotein 1 is a protein in the body to which antibodies against cardiolipin bind. Antibodies to beta2 glycoprotein 1 can also be measured. A person can be positive for antibodies against cardiolipin and negative for anti-2 GPI and vice versa.
The reasons for the appearance of the increase
Antiphospholipid antibody syndrome (commonly referred to as antiphospholipid syndrome or APS) is an autoimmune disorder that is present primarily in young women. Those with APS that make abnormal proteins are called antiphospholipid autoantibodies.
This leads to abnormal blood flow and dangerous clotting in the arteries and veins, problems with the developing fetus, and miscarriage. People with this disorder may be healthy or have an underlying condition, most commonly systemic lupus erythematosus (commonly called lupus or SLE).
Antiphospholipid antibodies, the analysis of which shows that women suffer from the disease 5 times more often than men, can be diagnosed up to 40-45 years old. Up to 40% of patients with SLE test positive for antiphospholipid autoantibodies, but only half of them develop thrombosis and miscarriages.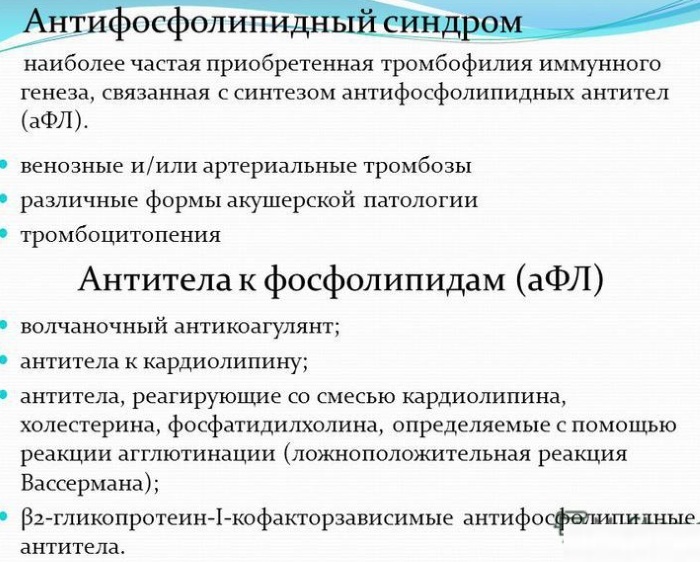
Like most autoimmune diseases, APS has a genetic component, although there is no direct parent-to-child transmission:
- Antiphospholipid antibodies are present in 15-20% of all cases of deep vein thrombosis (blood clots) and in 1/3 of new strokes occurring in people under the age of 50.
- Antiphospholipid antibodies are a major cause of recurrent miscarriages and pregnancy complications when no other cause is found.
- Diagnosis and treatment are very important. Once the disease is diagnosed, adequate therapy can prevent recurrence of symptoms in most cases.
- The mainstay of treatment is to prevent blood clots from forming with oral anticoagulants (blood thinners) or anti-platelet drugs.
Thrombosis risk factors must be addressed. These include diabetes, hypertension or high blood pressure, hypercholesterolemia or high cholesterol, obesity, smoking, estrogen therapy during menopause.
Symptoms of appearance and increase
Signs and symptoms of antiphospholipid syndrome may include:
-
Blood clots on your legs (DVT). Signs of DVT include pain, swelling, and redness. These clots can enter the lungs (pulmonary embolism).

- Repeated miscarriages or stillbirths. Other complications of pregnancy include dangerously high blood pressure (preeclampsia) and premature birth.
- Stroke. It can occur in a young person who has antiphospholipid syndrome but no known risk factors for cardiovascular disease.
- Transient ischemic attack (TIA). Similar to a stroke, a TIA usually only lasts a few minutes and does not deal permanent damage.
- Rash. Some people develop a red rash with a lacy, mesh pattern.
Less common signs and symptoms include:
- Neurological symptoms. Chronic headaches, including migraines.
- Dementia and seizures are possible when a blood clot blocks blood flow to parts of the brain.
- Cardiovascular diseases. Antiphospholipid syndrome can damage heart valves.
-
Bleeding. Some people have a decrease in the number of blood cells required for clotting. This can cause episodes of bleeding, especially from the nose and gums.

Also, signs may indicate the development of other pathologies that are associated with the primary syndrome of the disease.
Indications for research
Antiphospholipid syndrome occurs when the immune system mistakenly produces antibodies that greatly increase the likelihood of a blood clot. Antibodies usually protect the body from viruses and bacteria.
A therapist, rheumatologist or gynecologist may prescribe testing and indications for testing. Depending on the diagnosis and the cause of the disease, the specialist may be a laboratory therapist who then reads the results of the study.
Antiphospholipid antibody testing is used to determine the cause of:
- Inappropriate blood clot formation (unexplained thrombotic episode, excessive clotting).
- Periodic miscarriage.
- Low platelet count (thrombocytopenia).

- Long PTT test.
Depending on the person's signs and symptoms, medical history, the practitioner may prescribe several tests to detect the presence of antiphospholipid antibodies and help diagnose antiphospholipid syndrome (APS).
Testing for beta-2 glycoprotein 1 may be prescribed along with other antiphospholipid antibodies to detect their presence and provide the doctor with additional information. If an antiphospholipid antibody is detected, the same test / tests can be repeated after 12 weeks to determine if their presence is permanent or temporary.
How is it determined?
Anticoagulant lupus tests include partial thromboplastin activation time (aPTT), dRVVT, clotting time of kaolin (or silica) and PTT mixing tests Anti-beta-2 glycoprotein antibodies 1. The diagnosis of antiphospholipid syndrome is made by testing the blood of patients with blood clots or recurrent miscarriages for antiphospholipid autoantibodies (aPL).
Screening is done using three types of tests. They may differ due to differences in aPL. Each individual test cannot detect all possible autoantibodies, so it is highly recommended that they be used together. At least 1 of these tests must be positive and confirmed in 2 cases with an interval of at least 3 months.
The presence of only positive blood tests in the absence of a clot does not confirm the diagnosis of antiphospholipid syndrome. Testing can also be done to check for a person with an autoimmune disorder that can occur along with diseases such as lupus.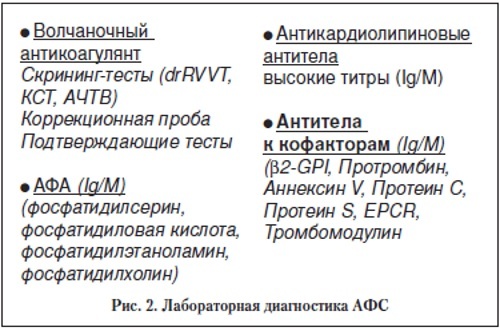
If a person with an autoimmune disorder tests negative for antiphospholipid antibodies, testing can be repeated to determine if the antibody has developed during the course of the disease.
Preparation and analysis
An analysis for testing antiphospholipid antibodies is carried out depending on the cause of the disease. APTT and PT show coagulograms, which are detected by tests of the effect of the presence of VA. The TNT mixed test is carried out according to the principle of screening and laboratory methods that help to detect lupus antibodies.
Therefore, in advance you need:
- Avoid taking medications that can interfere with the outcome. False positive test results can occur in people who take drugs such as quinidine, procainamide, phenytoin, and penicillin.
- Eliminate all symptoms and diagnosis of syphilis.
- Confirm or deny pregnancy. Its presence may distort the results when passing repeated tests.
- The patient is recommended to donate blood on an empty stomach.
When screening and analyzing hCG, it is undesirable to consume food and liquids. The selected test criteria must be monitored for 12 weeks, and after this period, a blood test can be repeated.
Decoding the results
Given that only 1 class of antibodies can be detected, the results will indicate the following:
| Increased concentration of IgM antibodies | Acute development of antiphospholipid syndrome. |
| Low concentration of M class antibodies | Rheumatoid arthritis or Sjogren's syndrome is diagnosed. Drug-induced lupus erythematosus, Lyme disease and syphilis can also be detected. |
| Checking for lupus hemostasis | When the number of antibodies fluctuates, there is no need to control them. The doctor prescribes the delivery of tests for re-examination. |
| Identification of several classes of antibodies | In this case, we are talking about the development of a severe form of APS. |
Antiphospholipid antibodies (analysis is carried out in any clinical laboratory) should be interpreted no earlier than 3-4 weeks after the delivery of the material. Care must be taken when interpreting the results of antiphospholipid antibody tests.
A negative result only means that the specific antibody being tested was not present during the test:
- Low to moderate levels of 1 or more antibodies may occur temporarily due to infection or drug, and may occur as the person ages. In some cases, a person may have 1 or more classes of immunoglobulins of a particular antibody, either present or absent in the blood. For example, a person may have significant amounts of IgG and IgM cardiolipin antibodies, or be only positive for the less commonly tested IgA cardiolipin antibody.
- Moderate or high levels of 1 or more antiphospholipid antibodies that persist with repeated testing after 12 weeks indicate the likely continued presence of this specific antibodies.
- If the tests indicate the presence of a lupus anticoagulant, and it persists with repeated testing, then it is likely that the person has a positive relationship to the anticoagulant of the disease. People who have 1 or more antiphospholipid antibodies and those who have been diagnosed with antiphospholipid syndrome, may be at risk for recurrent blood clots, miscarriages, and low platelet counts (thrombocytopenia).
- The test results cannot predict the likelihood of complications, type or severity, in a particular person. Some people will have many recurring problems, while others may never have any difficulty.
Temporary antiphospholipid antibodies can be seen in people with inflammation, autoimmune disorders, infections, or cancer.
When to see a doctor
If unexplained bleeding from the nose or gums, an unusually heavy menstrual period, bright red vomiting, or similar to coffee grounds, black, tarry, or bright red stools, or unexplained abdominal pain, see a therapist or family to the doctor.
He is obliged to issue a referral for testing. After receiving the results or while waiting for them, the patient should undergo an ultrasound scan and an initial examination by a rheumatologist and surgeon.
In some cases, you will need to go through an X-ray, visit a pulmonologist, as often clots (blood clots) force you to cough violently. In a normal state, young people, especially women, must take tests and analyzes once a year free of charge according to state quotas in the direction of a doctor.
How to bounce back
The need for long-term oral anticoagulant (blood thinning) therapy significantly affects the lifestyle of patients, creating the need for regular monitoring of the anticoagulant (blood thinning) effect and special attention paid to diet and situations with bleeding.
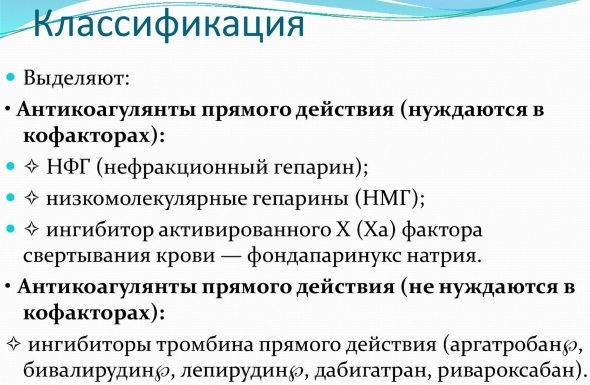
The use of new oral anticoagulants that do not require regular monitoring is being evaluated in ongoing clinical trials.
Correction of commonly accepted risk factors for thrombosis (diabetes, high blood pressure, high cholesterol, obesity and smoking) is mandatory for patients with antiphospholipid syndrome.
Estrogen therapy for birth control or menopause symptoms should generally be avoided with few exceptions in patients with a low risk profile, which should be assessed on a case-by-case basis case.
The current treatment for the prevention of obstetric manifestations is quite effective. Most women can have healthy children. Although antiphospholipid syndrome is an autoimmune disease, its diagnosis does not mean that the patient will develop another autoimmune disease.
As a treatment, it is prescribed:
- Procainamide - Doses of cortisteroids are regulated by a hematologist.
- Anticoagulant therapy is selected depending on the identified antibody.
- Plasmapheresis and rituximab (eculizumab) are given intravenously or orally if thrombin is to be inhibited.
The presence of phospholipid antibodies in some cases can be temporary if they have been detected in people who do not have detectable diseases. The course of treatment is prescribed by a hematologist or therapist.
Possible complications
Antiphospholipid antibodies (the analysis allows you to prescribe a therapeutic treatment) found in the blood indicate the presence of a disease. If left untreated, there is a risk of complications.
Depending on which organ is affected by the blood clot and how severe the blockage is blood flow in this organ, antiphospholipid syndrome can lead to irreversible damage or death organ.
Complications include:
- Renal failure This may be the result of decreased blood flow to the kidneys.
- Stroke. Reduced blood flow to a part of the brain can cause a stroke, which leads to irreversible neurological damage such as partial paralysis and loss of speech.

- Cardiovascular problems. A blood clot in the limbs can damage the valves in the veins that hold blood in the heart. This can lead to chronic swelling and discoloration of the lower extremities.
- Heart damage is another possible complication.
- Lung problems. These can include high blood pressure and pulmonary embolism.
- Complications of pregnancy. These can include miscarriage, stillbirth, premature birth, slow fetal growth, and dangerously high blood pressure during pregnancy (preeclampsia).
Rarely, a person can face relapses even when choosing the right treatment.
If the doctor has identified by analysis the presence of antiphospholipid antibodies, it is necessary to undergo a full course of examination and treatment. Otherwise, the risk of complications will lead to disruption of the work of the heart and blood vessels, which will entail untreatable diseases, up to and including death.
APS video
Diagnostics of the antiphospholipid syndrome:



