Content
- General characteristics of the disease
- Reasons for the appearance
- Symptoms and Signs
- Infected or not: transmission routes
- Classification of infiltrates
- Round
- Cloud formation
- Developing as caseous pneumonia
- Tuberculous lobitis
- Periscissurite (regional)
- Basal
- Bronchobular induration
- Sizes and phases of development
- Resorption
- Sealing
- Decay
- Seeding
- Clinical features of the course of infiltrative pulmonary tuberculosis
- Diagnostic methods
- Differential differences
- Treatment principles
- Drug therapy
- Surgical intervention
- Folk remedies
- Recovery prognosis
- Possible complications
- Prevention methods
Tuberculosis is a severe infectious disease that predominantly affects the lower respiratory system. In 60-70% of cases, inflammatory foci (infiltrates) appear in the lungs, which consist of immune cells, fibrin and epithelium.
With a prolonged course and the absence of therapy, infiltrative tuberculosis is complicated by the formation of tuberculomas and cavities, caseous pneumonia and severe intoxication.

General characteristics of the disease
The infiltrative form of the disease is accompanied by the formation of exudative-inflammatory formations, in the center of which there is a disintegration of the lung tissue.
Reasons for the appearance
This pathology is always secondary. It develops when old infectious foci are reactivated or a large number of Koch's rods penetrate into areas of the lungs that have previously been in contact with this pathogen.
In the first case, the formation of an infiltration zone is a reaction to the progression of the disease. The surrounding tissues become inflamed and exudate begins to secrete.
In the second case, the formation of cell clusters is associated with an immune response to massive penetration of bacteria. In previously sensitized areas, an intense inflammatory process develops, which is accompanied by the formation of infiltrates.
Thus, this form of tuberculosis develops only in the presence of specific (secondary) immunity to the disease. The development of specific antibodies to the pathogen is possible either with constant contact with patients, or with the development of an infection inside the body.
Risk factors for primary and secondary infection are:
- alcoholic, nicotine and drug addiction;
- asocial lifestyle, poor sanitary and hygienic conditions;
- diseases of the endocrine, respiratory and cardiovascular systems (diabetes mellitus, bronchial asthma, emphysema, chronic pneumonia, cardiopulmonary insufficiency, etc.);
- occupational diseases associated with periodic poisoning with chemical reagents and other pollutants;
- stress;
- pregnancy;
- HIV, other forms of immunodeficiency;
- taking immunosuppressants;
- malnutrition, vitamin deficiency.
Primary and re-infection often occurs through constant contact with a patient with an open form of the disease. Infiltrative tuberculosis is diagnosed mainly in young patients.
Symptoms and Signs
The secondary process can be acute, asymptomatic or asymptomatic. The rapid development of pathology is observed in 15-20% of patients, gradual - in 50-60%, and latent - in 20-25%.
The infiltrative form of the disease is accompanied by the following patient complaints:
- fever (the temperature remains in the range of + 38... 38.5 ° C for 2-3 weeks);
- wet cough, hemoptysis;
- increased sweating;
- sleep disorders;
- muscle soreness, feeling of weakness;
- general weakness, fatigue;
- weight loss, loss of appetite.
Asymptomatic forms of pathology can manifest with massive pulmonary hemorrhage.

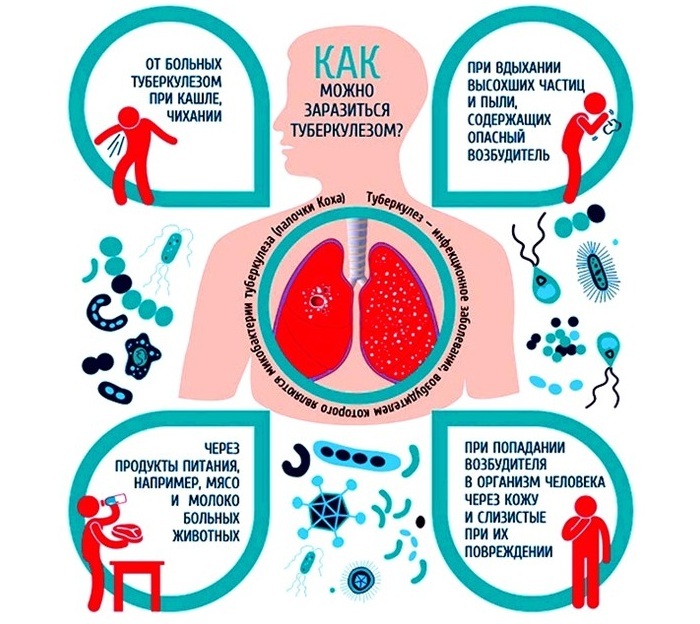
Infected or not: transmission routes
A patient with a secondary form of the disease is contagious at any stage of the development of infiltrates. Together with sputum, active mycobacteria are released, which remain on household items and penetrate into the lungs of other people with close contact.
Infection occurs mainly by airborne droplets - when coughing, sneezing, talking. Koch's wand can also be transmitted through everyday contact: through personal hygiene items, dishes, bedding, etc. On furniture, fabrics, books and clothes, it remains active for up to 5-6 months.
When living together, infection can occur through airborne dust. In dried drops of sputum, which mix with particles of epithelium and dirt, mycobacterium survives up to 1 year.
In street dust with diffused light, the pathogen remains for 1.5-2 months. If the phlegm dries up in direct sunlight, the mycobacterium dies.
Important information: The clinical picture of the development of cavernous pulmonary tuberculosis in adults
The following routes of infection are less common:
- alimentary (through food - raw meat, milk, cheese, etc.);
- through infected water;
- transplacental (from a sick mother to a fetus).
In young children, infection with Mycobacterium tuberculosis can occur through the conjunctiva of the eyes.
Classification of infiltrates
The type of infiltration is determined by its shape and density on an X-ray. Formations can be localized (broncho-lobular, rounded, basal) or extensive (caseous, lobar, marginal).
Round
Rounded infiltrates have uniform density, clear contours and small size. With the progression of the disease, an area of decay appears in the center of education. Round lesions are localized mainly in the uppermost segment of the lungs (S1) near the clavicular fossa.
The egg-shaped formation can have an elongated "track", which gives it the resemblance to a tennis racket. The walls of the bronchus near the affected area are always thickened.
Rounded infiltrates occur with tuberculosis against the background of a moderate decrease in immunity.

Cloud formation
Cloud-like foci are indistinct, indistinct contour and large in size. On the X-ray, they look like areas of weak darkening with several areas of decay.
Such formations are prone to rapid progression. In the affected lung tissue, foci of necrosis and cavities (cavities) quickly appear.
A cloud-like formation is formed in severe immunity disorders. In the development of inflammation, exudative and dystrophic phenomena predominate. Most often, several segments of the lung are involved in the process.
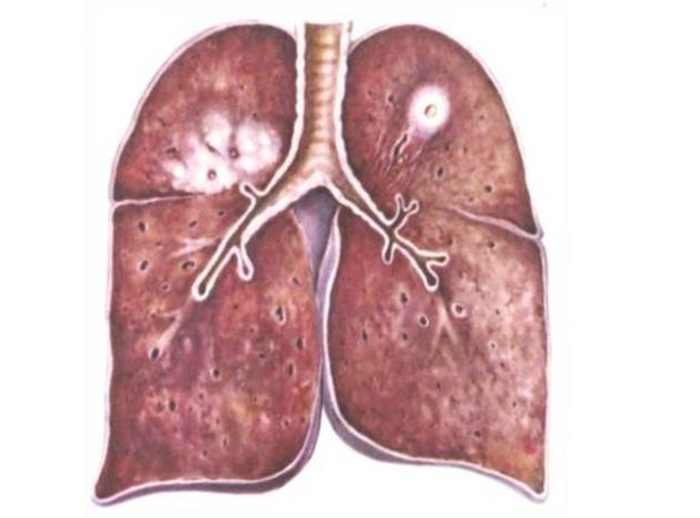
Developing as caseous pneumonia
With an unfavorable course of the disease, lobar caseous pneumonia is diagnosed. The process captures 1 or more lobes of the lungs. In the picture, the infected area is manifested by uneven darkening with 1 or more foci of decay.
The development of infiltrates is accompanied by extensive necrosis of the lung tissue, which worsens the prognosis. In most cases, caseous pneumonia develops against the background of immunodeficiency states: HIV infection, pregnancy, diabetes mellitus, etc.

Tuberculous lobitis
If, with secondary tuberculosis, the whole lobe of the lung is affected, then the infiltration is called lobit. In this case, a large area of darkening with uneven density and foci of decay is determined on the roentgenogram. In most cases, the process involves the upper segments of the lung.
Pulmonary tuberculosis develops against the background of severe immune disorders. Mycobacteria spread from the decay cavities through the bronchi and blood.

Periscissurite (regional)
Periscissuritis is an interlobular (marginal) infiltrate. It is located in the main or accessory gap between the pulmonary lobes, often involving the pleura. In the pictures, the interlobar lesion has an elongated shape and 1 clear edge.
Periscissuritis develops with severe immunity disorders.
Basal
The cause of the formation of basal infiltrates are not foci of infection in the lungs, but tuberculosis of the intrathoracic lymph nodes. Exudative accumulations at the roots of the lungs are most typical for children. Basal formations are less prone to decay than cortical formations.
For differential diagnosis of pulmonary and root infiltrates, a multi-axis X-ray examination is required.

Bronchobular induration
Bronchobular formations are small and localized in the upper segments of the lungs (S1, S2). The outbreaks can be polygonal, triangular or circular.
Lobular seals develop with normal immunity, therefore, exudative rather than destructive processes prevail. Areas of tissue destruction are small or punctate. In some cases, cords (adhesions) appear in the affected areas, affecting the costal pleura.
If there are several infiltrates, then they gradually merge, forming a seal with uneven edges and a decay area in the center.

Sizes and phases of development
Tuberculous infiltrates can be small (up to 2 cm), medium (2-4 cm), large (4-6 cm) and extensive (more than 6 cm). After the formation of an inflammatory focus, its resorption, compaction or decay occurs. The phases of development of an infiltrate are determined by its type and size.
Important information: The clinical picture of the course of fibrocavernous pulmonary tuberculosis
Resorption
In this phase, partial or complete resorption of the infiltrate occurs. The resulting cavities are covered with scars, and the release of exudate and necrotic masses decreases or stops. At this stage, the patient's condition improves dramatically.
Sealing
In the phase of compaction, the infiltrate is encapsulated in a dense fibrous membrane. In most cases, this occurs when the lesions are small.
Termination of the inflammatory process before the stage of decay reduces the infectiousness of the patient, but worsens the prognosis. A breakthrough of the fibrous capsule and a relapse of the disease can happen at any time.
Decay
The disintegration of the infiltrate is accompanied by the destruction of the infected lung tissue and the formation of cavities. In this phase, the most active release of the pathogen into the external environment occurs. The patient should be kept separate from healthy people and receive medical attention.

Seeding
At the stage of seeding, small foci of infection are formed around the main infiltrate. This phase can be virtually asymptomatic or with slight temperature fluctuations. As the disease progresses, the formations merge, and the patient's condition deteriorates sharply.
Clinical features of the course of infiltrative pulmonary tuberculosis
For extensive lesions, an acute manifestation is characteristic, and for local infiltrates - an erased or asymptomatic course.
Various types of formations have the following clinical features:
- broncho-lobular and round infiltrates - asthenovegetative syndrome, soreness of the shoulder muscles, a slight lag in the affected half of the chest during breathing, pleurisy may develop;
- cloudy formations, periscissurite - severe intoxication (depending on the size and stage of the process), wet cough, in some cases - hemoptysis;
- lobit - a strong productive cough, severe intoxication with temperature fluctuations due to the appearance of foci of dropout.
With the development of infiltrates of the type of caseous pneumonia, there is an intense wet cough, fever (up to + 40... 41 ° C), chills, severe weakness.
Diagnostic methods
The following methods are used to diagnose infiltrative tuberculosis:
- radiography;
- CT, MRI;
- tuberculin test;
- general and biochemical blood test;
- bronchoscopy with bacteriological examination;
- ELISA, PCR of blood and sputum;
- quantiferon test;
- auscultation, chest percussion, etc.

Differential differences
Differential diagnosis of the disease is carried out with croupous and atypical pneumonia, Leffler's syndrome, actinomycosis, candidiasis of the respiratory system, cancer and pulmonary infarction.
Differential diagnosis of tuberculous infiltrates
| Disease | X-ray signs | Symptoms | Changes in blood count | Other signs |
| Tuberculosis | Homogeneous or inhomogeneous shadow with foci of decay | Fever, wet cough of blood, signs of intoxication | Increased ESR, shift of the leukocyte formula to the left (up to 30% of stab neutrophils), with severe course - anemia | Positive Mantoux reaction |
| Croupous pneumonia | Homogeneous infiltration of a lobe or segment, predominantly in the lower or middle lung | Sternum pain, weakness, shortness of breath, wet cough, rusty phlegm | Leukocytosis, increased ESR, shift of the leukocyte count to the left | Rapid improvement in the condition against the background of antibiotic treatment |
| Lungs' cancer | Volumetric homogeneous formation, atelectasis, bronchial filling defect, coarse cords | Cough (dry or with little phlegm), hemoptysis | Increased ESR, anemia, moderate leukocytosis | Enlargement of supraclavicular and intrathoracic lymph nodes with metastasis |
| Eosinophilic infiltrate (Loeffler's syndrome) | One or more infiltrates with a vague or rounded outline | Cough with bright yellow sputum, slight intoxication | Eosinophilia (10-70% of leukocytes) | Positive allergy test or parasite test |
| Lung infarction | Triangular darkening with apex at the root of the lung, localized in the middle or lower lobe | Shortness of breath, tachycardia, fever, cough, acute chest pain, hemoptysis | Hypercoagulation | Overload of the right heart on the ECG |
| Actinomycosis | A dense infiltrate that occupies a lobe or segment of the lung is more often localized in the lower part of the lung | Cough, fever, hemoptysis, sternum pain | Increased ESR, intense leukocytosis | Is accompanied by thickening of the pleura and bone damage |
| Candidiasis | Infiltrate with vague contours, often in the lower or middle lobe of the lung | Cough with a small amount of secretion, temperature in the range of + 37... 39 ° С | Agglutination when mixed with an anti-Candida antibody preparation | Often combined with fungal stomatitis, pharyngitis, laryngitis, or glossitis |
Important information: The clinical picture of the development of tuberculous pleurisy in humans
Treatment principles
For the treatment of the infiltrative form of tuberculosis, medication (conservative) and surgical methods are used. Folk remedies can be used to increase the general tone and relieve coughing.
Drug therapy
The following drugs are prescribed for the treatment of tuberculosis:
- antibiotics (Rifampicin, Isoniazid, Ethambutol, etc.);
- immunomodulators;
- glucocorticosteroids;
- vitamins, antioxidants;
- mucolytics;
- hepatoprotectors.
With a correctly selected medication course and adherence to the rules of treatment, clinical symptoms disappear after 3-4 weeks. Resorption of foci and cessation of bacillic excretion occurs 3-6 months after the start of therapy.

Surgical intervention
With extensive necrosis, surgical treatment is prescribed. Depending on the size of the lesion, a segment, lobe or whole lung is removed.
In some cases, interpleural thoracoplasty is prescribed. In this operation, not only the affected segments of the lung are removed, but also several ribs.
The main indications for surgical intervention are bleeding in the cavity, purulent pleurisy and fibrous-cavernous tuberculosis, which cannot be stopped by artificial pneumothorax.
Folk remedies
Traditional medicine can be used in addition to conservative and surgical treatments.
The most effective home remedies are:
- medicinal herbs (knotweed, birch buds, dill, nettle, echinacea, wild rosemary, etc.);
- beekeeping products (propolis, bee bread, honey);
- animal fats (fish, badger, bear, etc.);
- aloe;
- garlic;
- mummy.

Recovery prognosis
The prognosis for infiltrative tuberculosis can be:
- favorable (complete resorption);
- relatively favorable (partial resorption, calcification of a caseous focus, formation of a scar or tuberculoma);
- unfavorable (the formation of large cavities with caseous-purulent contents, the development of complications).
The prognosis of recovery depends on the location, shape and size of the infiltrates. With small formations, complete resorption occurs, and with large and extensive seals, the development of pneumonia, the formation of cavities and tuberculomas.
The right-sided process is characterized by a low risk of cardiac dysfunction and complications during surgery. From the upper segments of the left lung, the infection can penetrate the vessels of the myocardium. This provokes the development of arrhythmia, myocarditis and cardiomyopathy.
If the foci are located in the lower segments of the lungs, the removal of caseous masses is complicated. With the progression of the disease, new infiltrates are formed, bronchial tuberculosis develops. The defeat of the lower lobes is observed in only 3% of patients. The prognosis of recovery in such patients is unfavorable.
Possible complications
The infiltrative process can be complicated:
- caseous pneumonia, fibrous-cavernous tuberculosis;
- cardiomyopathy;
- tuberculous meningitis;
- respiratory failure, lung atelectasis, pleurisy, pneumothorax;
- sepsis.
Prevention methods
To prevent the development of secondary tuberculosis, it is necessary to undergo fluorography annually, observe hygiene rules, eat well and treat chronic infections in a timely manner.
With immunodeficiency and constant contact with patients, regular revaccination with BCG vaccination is important.



