Content
- What is hysteroscopy in gynecology?
- Types of hysteroscopy
- Indications and contraindications
- Preparation for hysteroscopy
- How is the procedure going, does it hurt
- Possible complications from hysteroscopy
- How is recovery after hysteroscopy
- When can you plan a pregnancy after hysteroscopy of the uterus
- Video about office hysteroscopy
Recently gaining very popular hysteroscopy the uterus of the office variety, which allows you to quickly and efficiently find the pathological process with its subsequent elimination. The main advantage of the procedure is the minimal risk of complications and high efficiency.
What is hysteroscopy in gynecology?
Office hysteroscopy is a hysteroscopic type of examination that is often performed on an outpatient basis. In modern practice, this type of diagnosis has become quite widespread.
The main stages of office hysteroscopy:
- Treatment and disinfection of the external organs of the reproductive system.
- Introduction of the hysteroscope device.
- Comprehensive examination of the inner walls of the uterus, the canal and the vagina itself.
- Collection of tissues required for further research.
- Elimination of any pathological neoplasms, if any.
Office hysteroscopy is characterized by the use of equipment with a diameter not exceeding 5 mm, which greatly simplifies the intervention, and also reduces the risk of developing severe complications. In addition, the doctor can use other tools with which a biomaterial is taken, polyps are removed, or a pathological substance is removed.
The main advantages of this type of intervention include a reduced risk of complications, the possibility of effective and rapid examination of the uterine canal, as well as a relatively high speed of conducting, - the procedure most often lasts 10-15 minutes
In addition, hysteroscopy can be used before artificial fertilization of an egg or after unsuccessful conception attempts. This allows you to detect the main pathological processes that affect the inability to get pregnant.
Types of hysteroscopy
In gynecological practice, a surgical, control or diagnostic type is distinguished hysteroscopy, each of which has its own advantages and disadvantages, and is also characterized by a number of indications.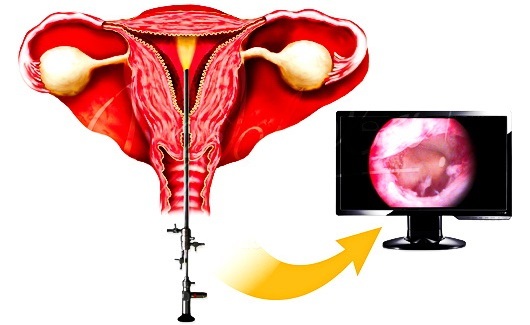
If hysteroscopy is performed for diagnostic purposes, the doctor uses a special device that is supplied with a fiber optic cavity. One part of the device is inserted into the internal cavity of the uterus, bypassing the vagina, while the second is held by the doctor with his hand. The device is capable of displaying a high-quality image on the display, which makes it possible to better assess the structure of the organ and identify the pathological process.
The surgical-type hysteroscope has built-in equipment that allows it to interact with the environment. Under the close supervision of optical devices, the gynecologist can eliminate various defects or pathologies observed on the inner walls of the uterine canal.
The device of the hysteroscope has clear advantages that distinguish it against the background of similar methods of diagnosis and therapy:
- the absence of a high expansion of the uterine canal, due to which the risk of degenerative changes in the uterus is significantly reduced, both in diagnosis and in treatment;
- a rather low probability of damage to the tissues of the mucous membrane, since any manipulations are accompanied by control through the display;
- the absence of any painful sensations during the study. The patient may experience only slight discomfort during the expansion process.
The ability to visually control the ongoing procedure using a computer screen allows the doctor to minimize the risks of any complications, as well as eliminate unwanted defects. The result is fast healing of the endometrium.
Indications and contraindications
Office hysteroscopy is a diagnostic procedure aimed at identifying various pathological conditions in the uterus, due to which the doctor can prescribe the most suitable and effective treatment. Timely diagnostics significantly reduces the risk of developing serious complications in the future.
The doctor who prescribes the procedure is most often a gynecologist who, after a personal conversation with the patient, which is accompanied by an initial examination, suggests the existence of one or another diseases.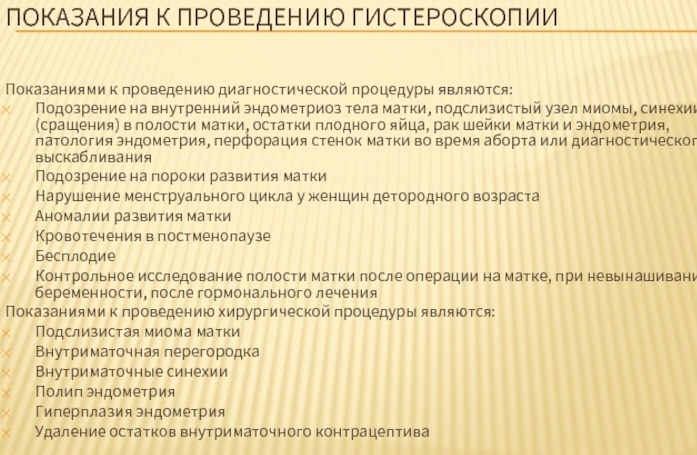
The main indications for office hysteroscopy:
- comprehensive examination after surgical or surgical interventions performed on the uterus, as well as during the course of hormonal treatment;
- the possibility of infertility due to a genetic or physiological component;
- the presence of bleeding in the postmenopausal phase;
- suspicions of the presence of abnormalities in the development of the uterine canal or pathological processes affecting the state of the endometrium or myometrium;
- obvious violations of the menstrual cycle;
- the presence of spontaneous termination of the pregnancy process;
- suspicions of the presence of foreign bodies in the uterine canal;
- the possibility of perforation or perforation of the inner walls of the uterus;
- complications arising in the postpartum period;
- scraping of the endometrium in order to diagnose the material obtained.
Hysteroscopy of office prostitution can be performed for the purpose of catheterization of the internal canals of the uterus or when removing large myomatous nodes. In this case, the doctor may resort to using another procedure - laparoscopy, which makes it possible to better recognize the pathological process.
In addition to the main indications, the procedure also has contraindications that must be taken into account in order to reduce the risk of developing dangerous complications during its implementation.
The most important contraindication is a diagnostic procedure during pregnancy, which can lead to miscarriage.
In addition, hysteroscopy is prohibited with the following symptoms:
| Sign | Description |
| Diseases of an infectious or viral nature. | Such a contraindication belongs to the group of absolute ones, because in its presence, there is a great risk of the infection spreading deeper through the canal. In this case, the procedure should be carried out only after the main infection has been eliminated. |
| Pathological processes of an inflammatory nature in the genitourinary system. | So, the study cannot be carried out in the presence of acute diseases, which are characterized by an inflammatory reaction. It is also prohibited during an exacerbation of chronic diseases. Diagnostics is used only after comprehensive treatment of the underlying pathological process. |
| Malignant formations in the cervix. | In this case, there is a rather high risk of developing cancers on the surrounding walls. This contraindication is due to the fact that hysteroscopy, although it allows you to better see the internal tissues organ, it also increases the spread of malignant cells into the abdominal region or uterine cavity pipes. |
| Uterine bleeding. | In this case, the research value of hysteroscopy is rather low due to the fact that the bleeding present significantly affects the analysis result. Here it is best to create the necessary conditions for the outflow of liquid matter and the elimination of the formed lumps. |
| Menstruation. | It is a relative contraindication due to the fact that during menstruation, the diagnostic value is also quite low due to a small overview of the inner walls of the organ. In this connection, hysteroscopy can be performed only 6-8 days after the menstrual cycle. |
| Pathological changes in blood clotting. | In this case, diagnosis is prohibited due to the high risk of blood loss, which significantly worsens the patient's condition. |
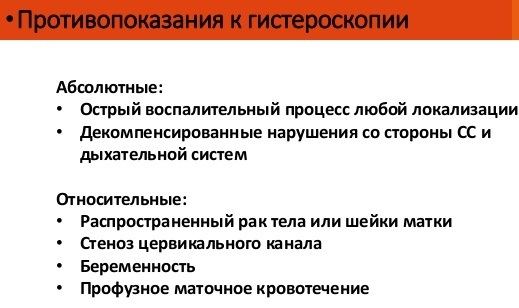
In addition to the above contraindications, the diagnostic procedure cannot be used in the presence of severe condition of the patient in the presence of somatic diseases, as well as in the case of narrowing of the inner neck uterus.
If the diagnosis is vital, the doctor can carry it out, despite the presence of certain contraindications. In this case, the main priority is placed on the life and health of the patient.
Preparation for hysteroscopy
Office hysteroscopy is a diagnostic procedure that requires a comprehensive examination. For this, laboratory, clinical, and instrumental methods can be used. Particular attention is paid to the so-called moral preparation, during which the doctor must explain the main purpose of the diagnosis, as well as point out its importance and the possibility of complications.
The main studies that can be prescribed before the direct carrying out of the diagnostic procedure:
- general and biochemical analysis of blood and urine;
- a study of the ability to coagulate blood or a coagulogram;
- quantitative serum sugar level;
- X-ray diagnostics of all organs of the thoracic region;
- ultrasound examination of the abdominal cavity, small pelvis, as well as the inner walls of the uterus;
- electrocardiogram;
- taking swabs from the inner walls of the vagina for examination for cleanliness;
The above studies can be ordered in order to detect and exclude pathological processes in the genital area, the presence of which is a contraindication to procedures.
If diseases have been detected, the patient is referred to the attending physician who can create an effective course of treatment. Diagnostics can be carried out both in stationary and in laboratory conditions. Only in the absence of contraindications, the doctor can conduct a hysteroscopy.
Also, before the procedure itself, the patient must adhere to some preparatory rules. For example, refuse to eat 8 hours before the diagnosis, carry out a cleansing enema, and also empty the bladder. In addition, it is recommended to reduce the consumption of alcohol and smoking, which can affect blood clotting.
Also, before direct intervention, a woman should speak with an anesthesiologist in order to provide important information about any allergic reactions. Thus, the doctor will be able to select the most effective drug and calculate the dosage pointwise.
How is the procedure going, does it hurt
Office hysteroscopy is a diagnostic procedure that should only be performed by an experienced doctor who specializes in the gynecological field. Often, diagnostics are performed in specialized clinics or general departments, in some cases it can be carried out on an outpatient basis.
For high-quality and safe diagnostics, the doctor must have the appropriate equipment. In addition to the chief physician, there must be an assistant and a resuscitator in the operating room. Before direct implementation, health workers should carefully examine the equipment, which implies an assessment of its functional state.
The main tool used for diagnostics is a hysteroscope. It is based on a special optical system designed for a comprehensive study of the internal canals of the uterus.
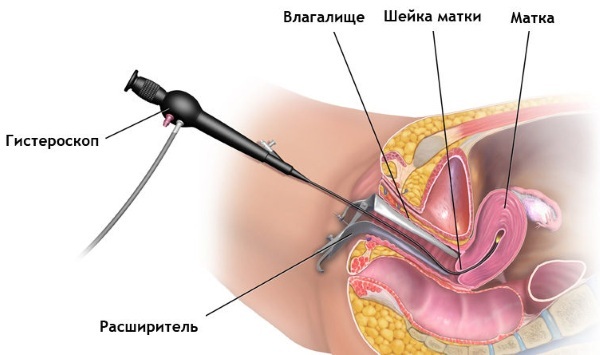
Depending on the intended intervention, the device can be equipped with additional tools:
- forceps to take a tissue sample;
- scissors;
- laser for effective and painless removal of pathologies or neoplasms;
- electrodes, which ensures good coagulation of internal tissues.
When performing surgical hysteroscopy, it is necessary to use general anesthesia, if the purpose of the procedure is diagnosis, a local anesthetic will be sufficient. The doctor then begins to open the inner cervix. The enlargement does not require a large diameter because the size of the hysteroscope is small.
With the help of a genital tube, a gas mixture or a specialized solution is introduced into the main cavity of the uterine canal, which additionally expand the walls and tubes. This allows you to better see each area of the lining of the uterus.
The doctor begins to gradually and carefully move the device inside the uterine canal, which is accompanied by a careful examination of all parts. In the presence of quality equipment, there is the possibility of a hundredfold increase, which makes it possible to better examine the cellular tissues of the endometrium.
In the case when hysteroscopy is performed only for diagnostic purposes, such manipulations are sufficient. However, if the procedure includes a treatment process, the necessary surgical equipment is inserted into the uterus with the help of a device, using which the doctor can eliminate the pathological process.
After completing any type of procedure, the gas mixture or solution is completely removed from the internal canals of the uterus. If there is such a need, the doctor can inject a medicinal substance into the organ. After that, the hysteroscope is gently removed through the vagina.
Possible complications from hysteroscopy
Given that hysteroscopy is a minimally invasive surgical intervention, the development of a complication is most often unlikely.
In some cases, the following symptoms may be present:
- increased bleeding;
- inflammatory processes in the endometrium;
- various menstrual irregularities;
- degenerative changes in the inner cervix, including its perforation;
- only partial elimination of pathological manifestations.
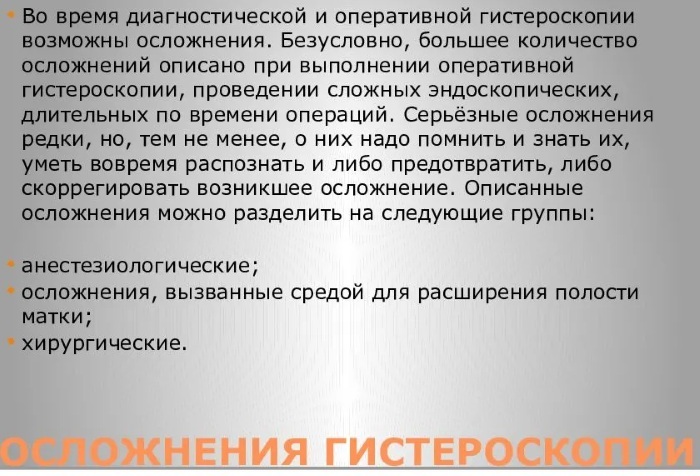
After surgical hysteroscopy, a slight deviation in the menstrual cycle is possible, which is explained by various disorders in the postoperative period, based on the fact that the body needs some time to recovery.
With a prolonged absence of menstruation, you should urgently consult your doctor, because such a symptom may indicate the development of dangerous complications in the future. Also, after diagnosis, the patient may feel pulling pains in the lower abdomen, since muscle fibers are able to respond to the device being inserted.
How is recovery after hysteroscopy
The rehabilitation period indirectly depends on which type of hysteroscopy was used. In the case of a diagnostic procedure, recovery is not necessary, so the patient will be able to do normal activities the very next day.
Surgical intervention in order to eliminate pathological signs should be accompanied by courses of antibiotic and antifungal drugs, which are prescribed strictly by a doctor.
Also, in the postoperative period, you should adhere to some recommendations:
- completely refrain from any sexual intercourse for a period previously agreed upon with the attending physician;
- do not use tampons for 6-12 days;
- refrain from visiting baths, saunas or swimming pools;
- avoid douching.
You should also pay special attention to the fact that physical activity during the rehabilitation period should be given minimal. If the basic recommendations for recovery are not followed, infection, organ injury, and heavy bleeding are possible.
Small bleeding is the norm with therapeutic intervention, which disappears within 3-4 days. In order for the recovery to go smoothly and quickly, the patient must follow a special diet. So, nutrition should not be deprived of vitamins and useful microelements. It is best to choose foods that are not heavy, with a slight laxative effect in order to reduce the risk of constipation.
3-5 days after surgery, the gynecologist must conduct a follow-up examination of the patient, in which the quality of healing of the surrounding tissues, as well as how effectively pathological neoplasms.
When can you plan a pregnancy after hysteroscopy of the uterus
After the hysteroscopy has been performed, it is necessary to wait a sufficient amount of time for the internal tissues of the uterus to fully recover. Therefore, the onset of pregnancy immediately after the procedure can be quite dangerous.
Despite the fact that most women believe that pregnancy after hysteroscopy is impossible, this opinion is erroneous. This is indicated by the fact that carrying out the intervention, on the contrary, only helps to fight infertility, as well as any other complications that are characteristic after the period of gestation.
The time allotted for pregnancy planning is displayed only by an experienced doctor who are individual in relation to a particular case.
Such a decision most often depends on many related factors:
- negative test result;
- the use of surgical or medical treatment;
- manifestation of various complications;
- the results of basic tests, including ultrasound and x-ray examination;
- lack of effectiveness in the treatment of the disease.
It is important to note that after an office hysteroscopy, pregnancy can be planned much earlier than after a therapeutic one - this is greatly influenced by the increased likelihood of complications. Such a minimally invasive intervention is able to reveal the main pathological process even at the initial stage of development.
Video about office hysteroscopy
Office hysteroscopy: