Content
- Topography of the superior vena cava
- Anatomy
- Structure
- Main functions
- Possible diseases and symptoms
- Congenital malformations of the superior vena cava
- Superior vena cava syndrome
- What doctors treat pathologies?
- Diagnostic methods
- Treatment
- Drug treatment
- Surgical methods
- Video about the superior vena cava
The structure of the upper vena cava (SVC), one of the main veins of the body, differs from the general anatomy of the veins in the absence of valves along the course of the vessel. The SVC carries blood to the right side of the heart, adjacent to the right atrium. There is no valve between it and the vessel.
Topography of the superior vena cava
Superior vena cava (the anatomy of the mediastinum involves a large number of vital organs in limited space) is surrounded on all sides by organs, pathologies of which can lead to squeezing:
| Organ | Position regarding ERW |
| Trachea | Left and back |
| The beginning of the aortic arch | At the point of exit from the heart bag |
| Right main bronchus, pulmonary artery, vagus nerve | Behind |
| Mediastinal pleura, right phrenic nerve | On right |
| Thymus | In front |
| Lymph nodes | Surround all over |
Anatomy
The superior vena cava, the anatomy of which is of great clinical importance, has a length of 5 to 8 cm and a diameter of 21 to 28 mm. The fusion of the left and right brachiocephalic veins form the SVC at level I of the right costal cartilage, from where it goes strictly from top to bottom, to the place where the III costal cartilage connects with the sternum, and flows into the right parts of the heart through atrium.
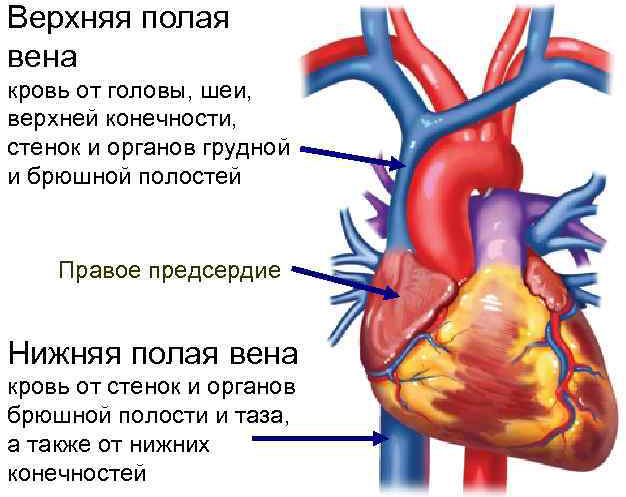
The SVC projection extends beyond the right border of the sternum by half its diameter. The pericardium of the heart captures the lower third of the vein, so that it partially lies in the cavity of the heart bag. The extrapericardial segment lies in the upper mediastinum, and the lower third is in the lower middle mediastinum.
Structure
The SVC enters the systemic circulation, which begins in the left ventricle and ends in the right atrium.
The vessel collects oxygen-poor blood from all organs of the upper body. The superior vena cava basin includes deep and superficial veins of the neck and head, deep and superficial veins of the arms, veins of the chest, namely: azygos and semi-unpaired veins, left and right brachiocephalic veins.
Main functions
The SVC carries venous blood to the heart. The blood of the SVC contains a lot of carbon dioxide in erythrocytes and little oxygen: the partial pressure of carbon dioxide in the blood is 41-51 mm Hg. Art., oxygen - 35-49 mm Hg. Art., and saturation (an indicator of saturation of hemoglobin with oxygen) is at the level of 70-75%. While in arterial blood, these indicators are 35-45 mm Hg. Art., 80-85 mm Hg. Art. and more than 95%, respectively.

Due to the low oxygen saturation, the blood in the vein is dark, cherry or dark purple in color. Venous blood is colder than arterial blood, contains less glucose and other nutrients, but contains more metabolic products (such as urea or creatinine). The acidity of venous blood is 7.36 versus 7.42 in arterial blood.
In medical practice, using special catheters, doctors gain access to large vessels: the femoral and subclavian veins, the internal jugular vein, and the superior vena cava.
The anatomy of the articulation of the superior vena cava with the right atrium allows for relatively safe insertion of a central catheter into the right atrium to measure central venous pressure. Normally, it should not rise above 4-5 mm Hg. Art. This study provides important diagnostic information for serious heart and lung conditions.

Using a central venous catheter in the SVC and other large veins, the following is performed:
- prolonged infusion of drugs;
- volumetric administration of blood products and blood substitutes during resuscitation;
- administration of medications that can damage smaller veins;
- parenteral nutrition.
Possible diseases and symptoms
With neighboring organs and understanding how this complex functions are the key to understanding the symptoms of diseases of the superior vena cava.
She is prone to pathologies, which are divided into two large groups:
- congenital malformations of the superior vena cava;
- kava syndrome.
Congenital malformations of the superior vena cava
Congenital malformations of SVC take on the most bizarre forms. Some do not have clinical manifestations and become an accidental finding when examining a patient.
Accessory or persistent left superior vena cava (LVCV) is present in 0.3-0.4% of people and accounts for 2 to 10% of congenital heart defects (CHD). Pathology makes itself known in the process of catheterization of the right half of the heart through the veins of the left arm.
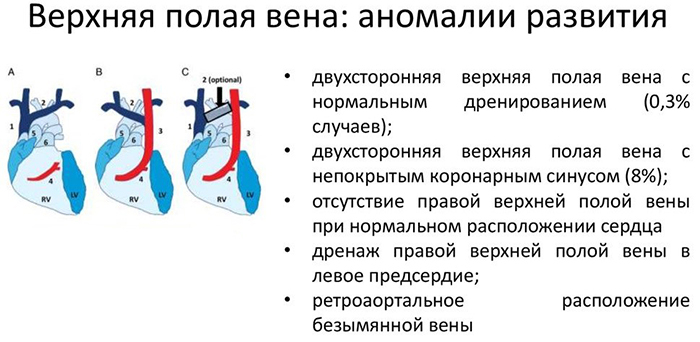
Then PLVPV can potentially lead to complications during manipulations on the cardiac conduction system, implantation of electrodes pacemaker or cardioverter-defibrillator, central venous pressure catheterization, connecting the device artificial circulation.
Violation of embryonic development is the main reason due to which the accessory left superior vena cava appears.
Anatomically, the fetus is different from the adult's body, because before birth it does not need pulmonary breathing: oxygen and nutrients enter through the umbilical veins, then blood flows through the umbilical arteries to placenta. Non-closure of the left anterior cardiac vein of the fetus and leads to the formation of PLVPV.
The left-sided superior vena cava (HDVC) occurs when there is a violation of the left anterior cardiac vein overgrowth: in 2% of cases, this is accompanied by obliteration of the vein of the same name on the right side. Thus, HDL remains the only one.
In 82-92% of cases, PLVPV flows into the right atrium and does not lead to hemodynamic disturbances, but it can associated with disturbances in the generation and conduction of an electrical impulse in the conducting system hearts.
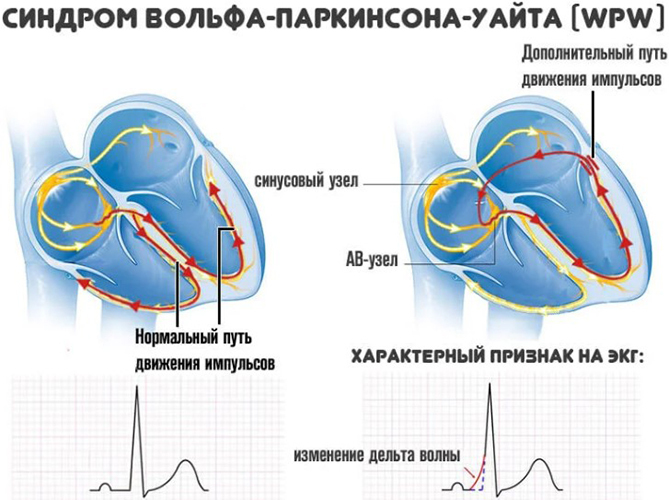
In this case, various types of heart blockages, supraventricular heart rhythm disturbances, Wolff-Parkinson-White syndrome (pathology, in which an electrical impulse generated in the right atrium reaches the ventricles prematurely through an additional abnormal bundle Kent).
This can manifest itself with symptoms such as:
- a feeling of discomfort in the area of the heart;
- a feeling of "falling out" of the heartbeats;
- attacks of an accelerated heartbeat;
- slow pulse, below 60 beats per minute.
There is an 18-20% chance that HDL is leading to the left atrium instead of the right.
In 4.4% of cases, the pathology is combined with other CHD:
- single atrium;
- non-closure of the Botallov duct;
- defect of the interventricular and / or interatrial septum;
- coarctation (sharp narrowing in a short section) of the aorta;
- Fallot's tetrad;
- pulmonary artery stenosis;
- abnormal pulmonary venous return - a pathology in which the pulmonary veins with arterial blood flow into the right heart.
Symptoms largely depend on whether HDL is combined with other defects and how severe the anomaly is.
Among the clinical manifestations are the following:
- pain in the region of the heart;
- accelerated heartbeat;
- shortness of breath, attacks of suffocation;
- a feeling of interruptions in the work of the heart;
- cyanosis of the skin and mucous membranes;
- deformation of the chest like a "heart hump";
- frequent dizziness, fainting;
- general weakness;
- deformation of the fingertips like "drumsticks";
- deformation of nails like "watch glass";
- lag in physical development, low weight, short stature;
- underdevelopment of bones, muscles, joints;
- poor appetite;
- fast fatiguability.
Superior vena cava syndrome
Superior vena cava syndrome (SVCV), or, as it is also called, cava syndrome, occurs when SVC blood flow is partially blocked from within a vessel or by external compression.
The causes of kava syndrome are divided into five large groups:
- compression of the SVC by adjacent organs, enlarged lymph nodes or proliferation of connective tissue;
- germination of a thin wall by malignant tumors;
- cardiovascular insufficiency;
- thrombosis;
- congenital stenosis.
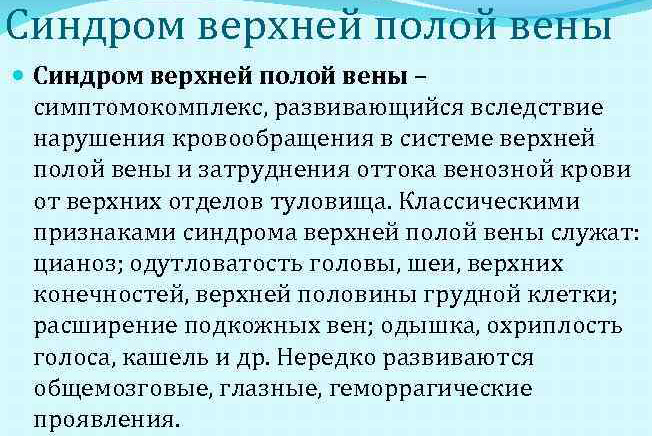
The symptoms of congenital SVC stenosis vary. A slight narrowing of the lumen of the vessel is asymptomatic, the detection of a defect will become accidental during examination or will remain undetected. Significant stenosis leads to a vivid clinical picture of cava syndrome from the first minutes of life.
SVC thrombosis can occur with serious injuries, with prolonged presence of the catheter in the subclavian vein or SVC, it can rarely occur spontaneously. Symptoms appear quickly, the body does not have time to adapt to the disturbance of blood flow and to engage collaterals (this is how the bypass paths of blood flow are called). This situation requires the immediate intervention of doctors.
When the SVC is compressed by neighboring organs or malignant tumors grow into the vessel walls, the clinical picture unfolds gradually. The human body has time to adapt to the violation of the outflow of venous blood from the upper half of the body and reveals collaterals, which, however, are not able to fully assume the functions of the SVC and replace her.
A patient with SVPV has a variety of complaints:
- headache and dizziness;
- fainting;
- seizures;
- swelling of the upper half of the body;
- drowsiness;
- dyspnea;
- cough;
- hoarseness of voice.
Some symptoms are caused by an underlying medical condition, not cava syndrome:
| Symptom | Frequency,% |
| Expansion of the veins of the neck | 66 |
| Dyspnea | 63 |
| Breast vein enlargement | 54 |
| Swelling of the face | 50 |
| Cough | 24 |
| Cyanosis (cyanosis) | 20 |
| Fullness of the face | 19 |
| Swelling of the shoulders | 18 |
| Chest pain | 15 |
| Dysphagia (swallowing disorder) | 9 |
The appearance of a person with a deployed SVPV is characteristic. Obstruction of blood flow through SVC opens collaterals and fills the vasculature with blood. The veins of the face and neck swell and do not subside even in the supine position, the neck swells (doctors call this symptom a Stokes collar). The superficial veins of the chest are full-blooded, the veins on the arms are clearly outlined, edema of the upper shoulder girdle may occur.
The blueness of the skin is especially visible on the face, the lips acquire a bluish-purple tint. The so-called Pemberton sign appears: if you raise your arms straight up, trying to touch your shoulders with your head, the patient's face will be bloodshot, reddened, the saphenous veins will sharply swell, within a minute there will be a feeling choking.
In case of acute cava syndrome, there will be no symptoms of "drumsticks" and "watch glasses" characteristic of chronic respiratory failure, but phalanges of the fingers can be deformed in a similar way during a long course of the underlying disease, if it is associated with cardiovascular failure. Cardiovascular failure can occur both as a complication of heart disease and become a complication of lung disease.

In some diseases, such as pulmonary fibrosis or chronic obstructive pulmonary disease, connective tissue grows in the tissues of the lungs. The resulting fibrosis blocks blood flow in the capillaries and leads to stagnation of blood in the lungs. The pressure in the small circle of blood circulation gradually increases, the load on the right parts of the heart increases.
The heart works in an enhanced mode, the myocardium of the right ventricle thickens, trying to pump blood into the lungs with great pressure. The enlarged right ventricle stretches the connective tissue ring, which forms the tricuspid valve that separates the ventricle from the atrium. This is how the tricuspid valve fails.
During the contraction of the right ventricle, part of the blood is pumped into the right atrium, which at this moment is relaxed and filled with blood from the SVC. For a while, the right atrium also builds up muscle mass to resist the volume pressure, but soon both (both the atrium and the ventricle) are depleted. The mass of the myocardium decreases, the walls become thinner.
The superior vena cava, whose anatomy does not provide for a valve between it and the right atrium, is facing increased pressure. The increased pressure, acting against the blood flow, gradually spreads to the entire SVC pool.
When SVCS is caused by tumors of adjacent organs or the invasion of a malignant tumor into the vessel wall, the mechanism of cava syndrome is simpler and similar to that in SVC thrombosis. A foreign object physically presses on the thin wall of the vein, partially or completely blocking its lumen and hindering the movement of blood. The pressure in the SVC system increases, symptoms of cava syndrome appear.
What doctors treat pathologies?
Independent SVC pathologies are treated by surgeons-cardiologists, vascular surgeons. Thrombosis requires the intervention of resuscitators, surgeons.
The main provocateur of SVPV is mediastinal oncology. In 75-80% of cases, this is small cell lung cancer, 10-15% are non-Hodgkin's lymphomas. Rare malignant causes include Hodgkin's lymphoma, leukemia, mediastinal vascular leiomyosarcoma, plasmacytoma, and metastatic cancer. Such cases require the intervention of oncologists to treat the underlying disease.
There are cases when SVPV provoked tuberculosis and syphilis. Doctors who will help with this: infectious disease specialists, dermato-vernerologists, and, if necessary, surgeons.
Diagnostic methods
Diagnosis of SVC pathologies begins with a survey and examination of the patient. A chest x-ray in two projections, frontal and lateral, and CT or MRI are indicated for all patients suspected of having superior vena cava syndrome.
With cava syndrome, 3D computed tomography with contrast is useful, thanks to which it is possible to see the exact boundaries of the tumor, the degree of damage to the mediastinal lymph nodes.

The need to distinguish SVC thrombosis from external compression requires the use of Doppler ultrasound scanning of the supraclavicular veins. Contrast phlebography is rarely done, but it is useful when you need to determine the length of the affected area of the vein. This information is needed to decide if surgery is possible.
Treatment
The superior vena cava, the anatomy of which is different from the structure of the rest of the veins, is treated in each case, depending on the damaging factors, the patient's condition and his vascular status. Traditionally, all methods of treatment are divided into therapeutic and surgical.
Drug treatment
With conservative methods of treatment, the following are used:
- systemic glucocorticoids;
- antiplatelet agents, anticoagulants;
- cytostatics;
- diuretics;
- radiation therapy;
- chemotherapy;
- antibiotics;
- thrombolytics;
- symptomatic treatment - pain relievers, antitussives.
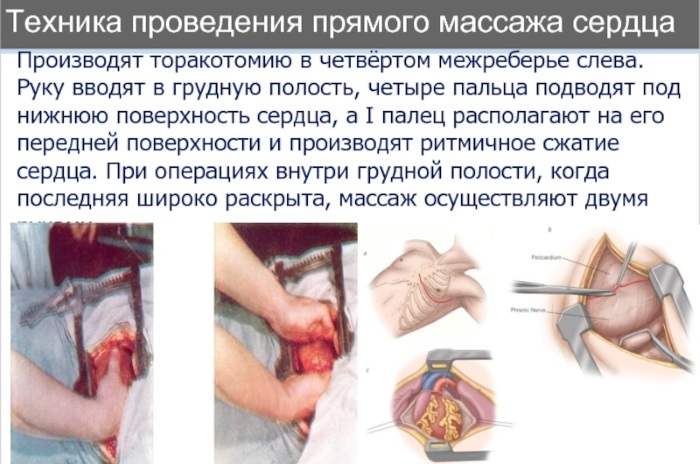
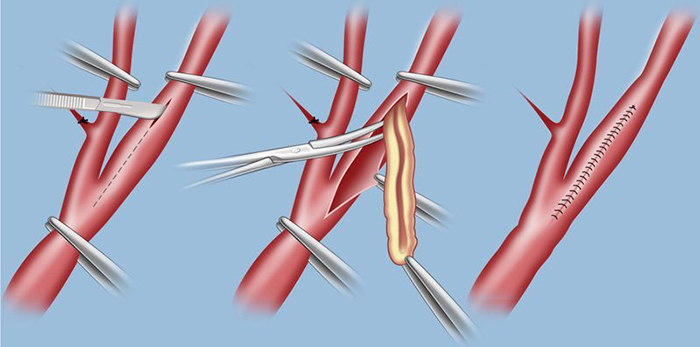
Surgical methods
The following operational techniques are used:
- intravascular stenting;
- intrathoracic or external bypass grafting;
- thrombectomy;
- percutaneous endovascular angioplasty and endoprosthetics;
- partial or radical resection of tumors;
The superior vena cava plays an invaluable role in the body, and its diseases are most often caused by the anatomy of the mediastinum. The close connection of organs and their influence on each other's functions means that treatment will require the advice of related specialists.
Video about the superior vena cava
Superior vena cava: formation, tributaries: