A biological test is carried out in all cases of blood transfusion. This is necessary to ensure the compatibility of the introduced components during transfusion. donor blood with the patient's blood and minimize the risk of adverse reactions.
Record content:
- 1 What is a biological sample and its features
-
2 Types of group affiliation that are checked during the trial
- 2.1 According to the AB0 system
- 2.2 Rh factor
- 3 Assessment of the suitability of blood for transfusion
- 4 Indications and contraindications for transfusion
- 5 Donor and recipient blood compatibility
-
6 Biological sampling and transfusion procedure
- 6.1 What the doctor should do before taking a sample
- 6.2 Where and how is the sample taken?
- 6.3 Transfusion algorithm
- 7 Do's and don'ts after a transfusion?
- 8 Patient's condition after transfusion
- 9 Blood transfusion video
What is a biological sample and its features
Blood transfusion or blood transfusion is a remedy that has saved millions of lives. But the result of a transfusion is not only positive, but also negative.
It is impossible to give a 100% guarantee that patients who received donor blood transfusions will not experience adverse reactions and complications. To prevent this from happening, samples are taken from the donor and recipient for individual blood compatibility.
A biological test for blood transfusion is performed at the beginning of the transfusion procedure. It protects the patient from complications caused by secondary group systems of red blood cells. They are represented by a large number of antigens.
Types of group affiliation that are checked during the trial
Upon admission of a patient who needs a biofluid transfusion, a primary study is performed on the R-factor and blood group. The procedure is carried out in clinics, diagnostic laboratories.
Blood components used for transfusion:
- erythrocytes;
- platelets;
- leukocyte mass;
- plasma.
All components must correspond to the ABO system group and the Rh factor that the recipient has.
According to the AB0 system
The AB0 blood group is the main blood classification system used throughout the world. This is the basis for comparing blood between donors and patients. A person's belonging to the AB0 blood group is determined through genetic inheritance. Some people inherit genes known as A. They code for antigens that trigger the rejection of blood cells.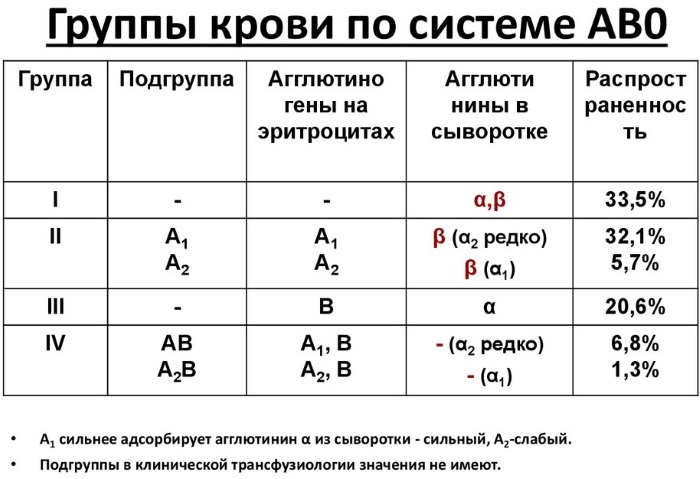
These people have type A blood. Others inherit the B genes, which code for the B antigen and are of the B blood type. It is also possible to inherit one copy of each antigen from the parents, resulting in AB blood. Some people inherit neither A nor B genes. They have group 0 blood in their bodies.
Testing technique for the AB0 system:
- a plate is taken, on one side of which the patient's data is entered, and on the other 2 drops of his blood serum are applied;
- a drop of donor blood is added to it (ratio 10: 1);
- the blood is mixed by periodic rocking of the plate, the laboratory assistant observes the reaction;
- in the absence of adhesion of the donor's erythrocytes, the laboratory assistant concludes that the blood is compatible in AB0 groups;
- if adhesion (agglutination) appears, this indicates their incompatibility.
Rh factor
The blood grouping system is complicated by the presence or absence of the Rh factor, another important component in the blood. The presence or absence of the R factor indicates that someone has "negative" or "positive" blood. Instead of dividing people by blood type into A, B, AB, or 0, doctors determine whether they are carriers of A-, A +, B-, B +, AB-, AB +, 0-, or 0 +.
The specificity of any organism is determined by the set of proteins or antigens that are part of any tissue. In the blood, erythrocytes are surface antigenic complexes.
One of these is the Rh factor or Rh antigen. Depending on this, all people are divided into carriers of the R + antigen and the R- antigen. With regard to donor compatibility, we are talking only about the erythrocyte mass and washed erythrocytes.
In the classical version, only blood with the same R-factor and group is considered fully compatible. But this rule does not always work in practice. In some situations, when an urgent transfusion is needed, there is no time to determine compatibility. The only salvation is the transfusion of whole blood or red blood cells in accordance with the principle of hypothetical compatibility.
Its options are shown in the table:
|
donor patient |
Group I, 0 (I) | Group II, A (II) | Group III, B (III) | IV group, AB (IV) |
|
I group 0 (I) |
compatible | incompatible | incompatible | incompatible |
|
II group A (Ii) |
compatible | compatible | incompatible | incompatible |
|
III group B (III) |
compatible | incompatible | compatible | incompatible |
|
IV group AB (Iv) |
compatible | compatible | compatible | compatible |
According to the table, conclusions can be drawn:
- People with the first blood group are universal donors, but they can only be recipients of the first blood group.
- People with the fourth blood group are universal recipients, although they can only be donors for people with the fourth blood group.
RH-factor compatibility in blood is determined by only two options, regardless of group membership: people with RH-negative blood can only be transfused with RH-negative blood. People with RH-positive blood can receive both RH-positive and RH-negative blood donors.
Assessment of the suitability of blood for transfusion
The donor blood is checked before the start of the transfusion by the same doctor who will carry out the transfusion procedure and trial actions.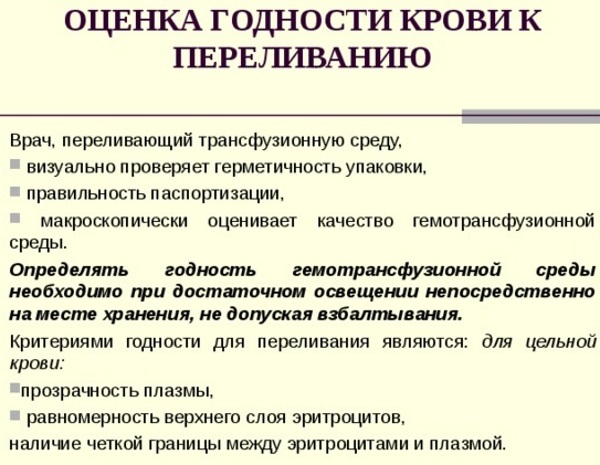
He should inspect the product, noting:
- expiration date of blood;
- availability and correctness of certification of the introduced product.
- the appearance and condition of the biological fluid.
Visually, the blood to be infused is divided into 3 layers:
- the top layer is transparent yellow plasma;
- the middle layer is a grayish white blood cell and platelet band;
- lower - red erythrocytes.
The three-layer structure is typical for whole blood intended for transfusion and is clearly visible in glass vials.
If erythrocyte blood components are intended for transfusion, then they can be in the form of a suspension, cryopreserved. Another commonly used component is plasma. It is presented in liquid form and dry, lyophilized.
Indications and contraindications for transfusion
There are many reasons why a blood transfusion may be needed.
Here are just a few of them:
- A complex operation or trauma in which there was a large loss of blood.
- Bleeding in the gastrointestinal tract due to an ulcer or other medical condition.
- For leukemia or kidney disease that causes anemia (a deficiency of healthy red blood cells).
- After radiation or chemotherapy.
- Blood disease or severe liver problems.
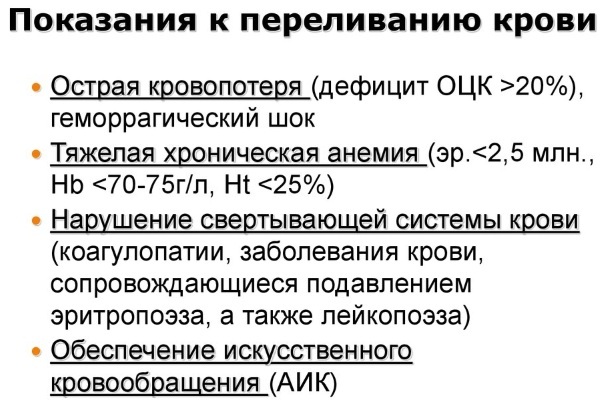
Indications for red blood cell transfusion:
- Acute sickle cell crisis (for the prevention of stroke).
- Large blood loss> 30% of the blood volume.
- Hemoglobin <7 g / dl.
- Symptomatic anemia.
Indications for transfusion of plasma products:
- Prevention of active bleeding in a patient on anticoagulant therapy before the procedure.
- Active bleeding.
- Intracranial hemorrhage
- Acute disseminated intravascular coagulopathy.
- Microvascular bleeding during massive infusion.
Platelet transfusion may be indicated to prevent hemorrhage in patients with thrombocytopenia.
An absolute contraindication to blood transfusion will be acute heart failure, which is accompanied by pulmonary edema and myocardial infarction. If a person received a traumatic shock, while losing a large mass of blood, then in this case, blood must be transfused urgently, despite the symptoms of the disease.
Relative contraindications include:
- functional disorders of the liver, kidneys;
- the consequences of damage to the walls of blood vessels in thrombosis and thrombosis;
- stage III hypertension;
- complex disorders of cerebral circulation;
- cross allergy;
- bronchial asthma;
- heart disease, myocarditis, septic endocarditis;
- miliary, acute tuberculosis;
- hemorrhagic vasculitis.
Donor and recipient blood compatibility
During the transfusion, the blood must be accurately matched. If a blood type A person is given blood from a blood type B donor, anti-B antibodies will adhere to the B antigens on the donor red blood cells that enter their body. This triggers a reaction that can be fatal. Hence, exact match is critical.
Cross-match is a pre-transfusion procedure to determine if the donated blood is compatible or incompatible with the recipient's blood.
Compatibility is determined by comparing different blood group systems, the most important of which are the ABO and Rh systems, or by direct testing for the presence of antibodies on donor tissue samples, or blood. Cross-matching reveals incompatibilities between donor and recipient that will not be visible when typing the blood.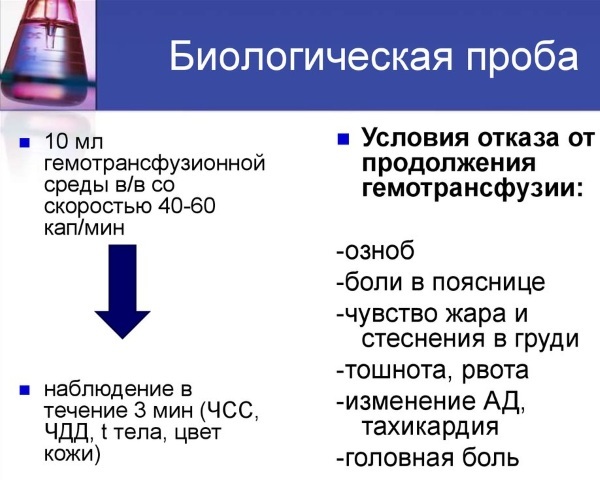
Basic cross-matching involves testing the patient's serum with donor cells to determine if whether the patient has an antibody that can cause a hemolytic transfusion reaction or a decrease in donor survival cells.
Biological sampling and transfusion procedure
A biological test for blood transfusion is performed at the beginning of blood transfusion. Despite being tested for AB0 and R-factor groups, doctors cannot always be sure of the full compatibility of the donor's and patient's blood. To exclude complications, another test is performed at the beginning of the transfusion - a biological one.
What the doctor should do before taking a sample
Before blood transfusion, the doctor performs the following actions:
- Indicates the presence of indications for transfusion of one of the blood components in the patient's record.
- Obtains the voluntary consent of the recipient or his representative to carry out the therapeutic procedure.
- Checks all the data on the label of the container with donor blood, which after the end of the procedure is included in the medical record.
- Records the results of the patient's blood test according to the AB0 system and the Rh factor.
- Checks the erythrocytes or total blood in the container according to the R-factor and the AB0 system, and records the results of the check in the medical record.
- Records both positive and negative results of a biological test carried out three times in the process of blood transfusion.
Where and how is the sample taken?
Blood transfusions, as well as immunohematological tests are carried out in a hospital, specialized clinics or outpatient clinics. To do this, you need an equipped room with natural light, a temperature of at least 16-25 ° С, as well as devices, instruments, consumables for analyzes and therapeutic operations.
A biological test for blood transfusion during blood transfusion is carried out in a hospital setting by the attending physician or the doctor on duty. In clinics, it is carried out inpatiently or outpatiently as prescribed by a surgeon, therapist or hematologist.
Transfusion algorithm
The container with the biological mass is kept in the refrigerator before the start of the procedure. Before use it is taken out and kept at room temperature for 30–35 minutes. By the time of transfusion, it should reach + 37 ° C.
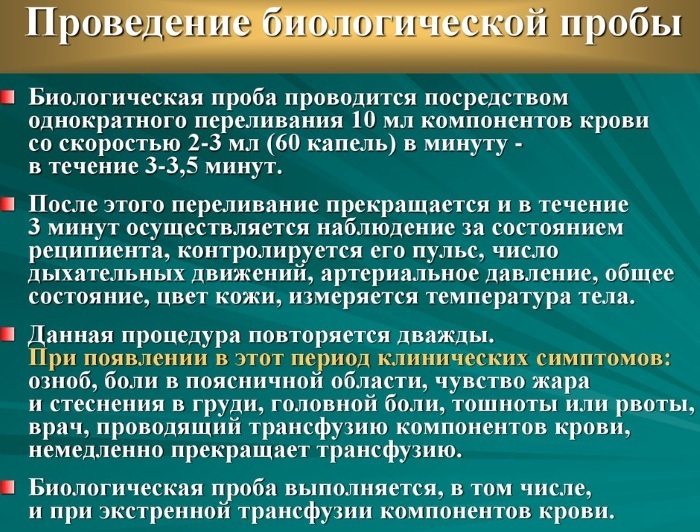 Before the start of the transfusion, a biological sample is necessarily made, while the doctor carries out a certain sequence of actions:
Before the start of the transfusion, a biological sample is necessarily made, while the doctor carries out a certain sequence of actions:
- 10 ml of blood transfusion fluid is injected drip. The rate of administration is from 40 to 60 drops per minute.
- Closes the clip on the intravenous system.
- Within 3 min. monitors the patient's condition.
During the observation, the following is checked:
- pulse;
- HELL;
- breath;
- Body temperature;
- discoloration of the skin, if any;
- general state.
The whole sequence of actions is carried out 2 more times. In the intervals between biological samples, the introduction of blood is not carried out.
After the introduction of a biological test blood, some patients develop alarming signals: chills, nausea, vomiting, a feeling of heat, tightness in the chest. If at least one sign is detected, an immediate termination of the entire transfusion procedure is required.
After stopping the therapeutic operation, blood is taken from the patient and sent to the laboratory, where the individual selection of the mass of erythrocytes is performed.
A biological test for blood transfusion is carried out regardless of the amount of injected blood, the rate of its introduction. The procedure is also carried out in the case of an emergency transfusion. If several doses of blood are administered to a patient, a biological test should be performed before each new dose.
A blood transfusion is a common medical procedure in which donated blood is given through a narrow tube placed in a vein in your arm. People receive blood transfusions for many reasons - surgery, injury, illness, and bleeding disorders.
Blood has several components, including:
- Red cells carry oxygen and help remove waste.
- White cells help the body fight infections.
- Plasma is the liquid part of blood.
- Platelets help the blood clot and stop bleeding.
The transfusion provides the part of the blood that is needed, and most often red blood cells are transfused. Whole blood containing all the parts is often given, but whole blood transfusions are not common.
For the introduction of erythrocyte mass in medical practice, other ways are used: intra-aortic, intraosseous, intra-arterial. The donor container with a small amount of biological fluid should be kept for 48 hours after the procedure.
Do's and don'ts after a transfusion?
A patient who has received a dose of blood in a hospital should within 2 hours. observe bed rest. The attending physician is observing him at this time. The recipient is measured hourly blood pressure, body temperature.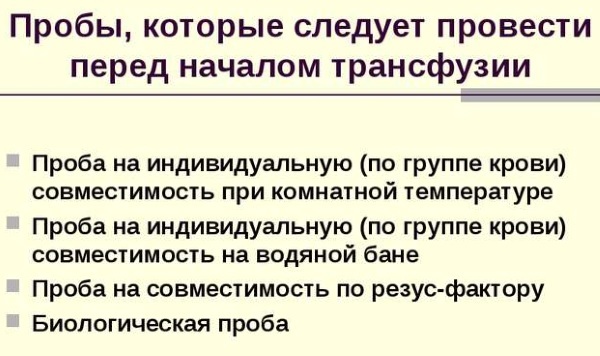
The presence of urine is monitored in the form of an hourly volume and a change in its color is recorded. A reddish color in the presence of transparency indicates the destruction of erythrocytes and the development of hemolysis. The next day, the patient undergoes a general urine and blood test.
In the case of blood transfusion in a clinic, the patient after the end of the procedure must be under medical supervision for at least 3 hours. In the presence of stable blood pressure and pulse, normal urinary function, and the absence of adverse reactions, the patient is released from the clinic.
After a blood transfusion, most people feel great with mild side effects. In rare cases, patients do not respond well to transfused blood during the procedure. In such cases, the process is interrupted and the person is provided with medical assistance. A thorough examination before transfusion is the best way to avoid a bad reaction.
Patient's condition after transfusion
In the vast majority of cases, people can resume normal activities after a blood transfusion, including eating, drinking, and taking all existing medications.
Most people can return home soon after a transfusion, unless the underlying medical condition requires a hospital stay. Patients should be aware of the signs of an adverse reaction and seek immediate medical attention if necessary.
It is important that the healthcare provider performing the transfusion performs pre-procedure screening and closely monitors the patient during the process. Reactions are more likely early in the transfusion, although they can sometimes occur later. Acute reactions can be life-threatening if not treated immediately.
Acute hemolytic reactions occur when incompatible red blood cells are injected into a patient. This is more often due to errors in obtaining or labeling group samples and antibody samples, or inability to perform the necessary checks at the patient's bedside prior to the administration of blood.
Signs and symptoms of erythrocyte incompatibility:
- Pain at the cannulation site.
- Pain in the chest, back, or abdomen.
- Hypotension / hypertension.
- Tachycardia.
- Feverish condition.
- Bleeding
- Collapse.
- Hemoglobinuria.
With platelet infusion, complications are possible if contaminated substances are injected.
Common signs include:
- feverish condition;
- tachycardia;
- collapse;
- acute lung injury caused by transfusion.
Complications of transfusion of plasma containing antibodies of white cells occur within 6 hours after transfusion and include:
- unproductive cough;
- hypotension;
- acute shortness of breath;
- hypoxia.
Allergic reactions usually occur early in the transfusion, and symptoms include:
- hypotension;
- bronchospasm;
- pain in the chest, abdomen;
- shortness of breath;
- nausea, vomiting;
- hives;
- redness of the skin;
- conjunctivitis.
Serious allergic reactions may occur, anaphylactic shock, in which the patient cannot breathe normally, and heart problems may begin. The post-transfusion response is the response of the immune system to donated blood. It can happen immediately or much later, and it can be mild or severe. The delay in reaction after the procedure can last for 3-10 days.
Seek medical attention if any of the following symptoms appear:
- double vision, headache;
- dizziness, a feeling of impending fainting;
- nausea, diarrhea, or abdominal cramps;
- purple spots on the body in the form of dots;
- dizziness and weakness about 7 days after the procedure;
- sweaty and cool skin;
- blue lips;
- yellowing of the skin and whites of the eyes.
Medicines will help improve the condition:
- Antihistamines can help reduce itching and swelling if you have a mild allergic reaction.
- Steroids can be taken to prevent inflammation.
- Fever medications will help improve the condition.
- Diuretics can help you get rid of excess fluid.
The medications you take should be agreed with the doctor who performed the blood transfusion in advance.
Blood transfusion helps restore blood volume, activate prothrombin, increase blood flow, help the body resist anoxemia, and improve defenses and disease resistance. In order for the blood transfusion procedure to pass without complications and cause no further reactions, doctors conduct a serious test in the form of tests for the Rh factor, AB0 and biological samples.
Blood transfusion video
Reception leads. Blood transfusion:



