1 Clinical picture
Acute pancreatitis is a condition dangerous to human life, associated with damage to the pancreas and destruction of adjacent tissues, sometimes distant organs. In European countries, the most common cause of acute pancreatitis is gallbladder( cholecystitis) and bile duct disease, alcohol abuse, which together account for about 80% of cases.
Do you have gastritis?
GALINA SAVINA: "How easy is it to cure gastritis at home for 1 month. A proven method is to write down a recipe. ..!"Read more & gt; & gt;

Recommended to consult
- Diet for pancreas problems
- Causes and treatment of chronic gastritis in adults
- Symptoms and treatment of gastric cardiac insufficiency
- Effective agent for gastritis and stomach ulcer
Other factors that cause acute pancreatitis are operating and some diagnostic procedures in the abdominalcavity, trauma, viral and parasitic infections, toxic effects of certain drugs. The essence of the inflammatory process in acute inflammation of the pancreas is the release of trypsin, which initiates the activation of enzymes of elastase. It plays a special role in the process of tissue damage of this organ.
In addition, in acute inflammation of the pancreas involved endotoxins of the bacterial flora, they can seep into the bloodstream from the affected intestines. As a rule, the first symptom of acute pancreatitis is very severe abdominal pain, which appears suddenly in the upper abdomen on the left, sometimes with irradiation in the spine. There is nausea, vomiting and high fever up to 39-40 ° C.The abdomen is painful and tense, the intestinal peristalsis is weak due to intestinal obstruction. In a short time, shock develops, the activity of pancreatic enzymes - amylase and lipase - increases. Necrotic and hemorrhagic complications occur in the pancreatic parenchyma.
2 Proper nutrition
With the development of acute pancreatitis and cholecystitis during the first 3 days, you will need absolute starvation, the goal of which is to exclude stimulants that stimulate the secretory activity of the pancreas. Simultaneously, the permanent suction of its contents through the gastric food probe is used to prevent vomiting.

The time of entering the first courses after fasting is individual for each patient and must be adapted to the pathological process of the patient taking into account biochemical indices and the state of intestinal motility. Nutrition for pancreatitis and cholecystitis should contain porridge, rusks, then introduce a diet of cereal and fruit( 1-5 days), then enrich it with skimmed milk, cottage cheese, waffles, mashed potatoes. Food from cereals and fruits, gradually expanding, becomes a low-calorie diet, used for chronic pancreatitis. You can eat a small amount of yolk. Carbohydrates should mainly come from grain products.
-
 IMPORTANT TO KNOW! Gastritis? Ulcer? To have a stomach ulcer not turned into cancer, drink a glass. ..Read the article & gt; & gt;
IMPORTANT TO KNOW! Gastritis? Ulcer? To have a stomach ulcer not turned into cancer, drink a glass. ..Read the article & gt; & gt;
3 Chronic course of the disease
Chronic pancreatitis causes progressive, irreversible changes in the pancreatic parenchyma in the form of atrophy and fibrosis, as well as the gradual development of pancreatic insufficiency. Its pathogenesis has not been fully understood. The main causes of the onset of chronic pancreatitis include the consequences of recurrent acute pancreatitis, fibrosis, cholelithiasis and chronic inflammatory processes of the biliary tract, disease states that hinder the outflow of pancreatic juice and bile, peptic ulcer and alcoholism.
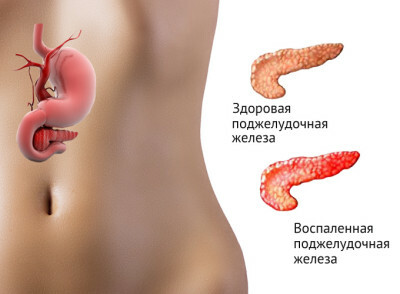
The inflammatory process in the pancreas region affects the deterioration of the work of this organ. There is a decrease in the secretion of bicarbonates and pancreatic enzymes, a decrease in the secretion of insulin, which in some patients leads to diabetes.
In chronic pancreatitis there is an increase in the secretion of hydrochloric acid, observed in patients with peptic ulcer of the duodenum. There is an acceleration of gastric emptying.
-
 Gastroenterologist. IMPORTANT: "I beg you, if you began to worry about abdominal pain, heartburn, nausea, do not in any way do gases. .."Read more & gt; & gt;
Gastroenterologist. IMPORTANT: "I beg you, if you began to worry about abdominal pain, heartburn, nausea, do not in any way do gases. .."Read more & gt; & gt;
Symptoms of chronic pancreatitis appear slowly. The abdominal pain predominates, which is localized in the epigastric region. It occurs after eating, often after drinking alcohol, lasting from a few hours to several days. Severe pain accompanies nausea, bloating, subfebrile temperature, weakness. Patients suffer from a lack of appetite, which, together with digestive and absorption disorders, contributes to weight loss, malnutrition, and even severe exhaustion of the body.
4 Recommendations
The diet for chronic cholecystitis and pancreatitis is aimed at alleviating pancreas and digestion. It is necessary to use preparations containing digestive enzymes. Violation of pancreatic secretion leads to poor digestion of all nutrients.
For chronic cholecystitis and pancreatitis, the products used should be easily digested, so a low-fat and low-calorie diet is prescribed. Dishes should be served in small portions while taking medications containing pancreatic enzymes. Eat small portions at regular intervals.
ADVICE FROM THE MAIN GASTROENTEROLOGIST
Korotov SV: "I can recommend only one remedy for the rapid treatment of Ulcer and Gastritis, which is now recommended by the Ministry of Health. .." Read testimonials & gt; & gt;
More fat in the diet is poorly absorbed and causes malfunctioning of the intestine. Protein is introduced into the diet based on a ratio of 1.0-1.5 g per kg of body weight.

The main source of energy are simple carbohydrates, obtained from foods that are poor in fiber. You can eat rusks, coarse bran, bread, cereals, cereals, small noodles, glucose, sugar, honey, jams and mashed potatoes, pitted fruit, mashed potatoes. The diet can be changed by introducing a small amount of egg yolk.
Patients with exacerbation of pancreatitis may need parenteral nutrition using intravenous injections containing amino acids, lipids, mineral salts and vitamins.
In many cases, there is a need for treatment with pancreatic lipase, which helps in the digestion of products containing fat. This protects the body from the deficiency of vitamins A, D, E, K and B1, B2, B6, which are fat-soluble.
In case of diarrheal symptoms it is recommended to eat vegetables and fruits in boiled or fried form. Thus, you can get rid of some fiber that increases diarrhea.
In dietary treatment, the most important is the elimination of harmful factors.
WE RECOMMEND!
For prevention and treatment of gastrointestinal diseases our readers advise Monastic tea. This unique remedy consists of 9 medicinal herbs useful for digestion, which not only supplement, but also strengthen each other's actions. Monastic tea will not only eliminate all symptoms of the gastrointestinal tract and digestive system, but will also permanently eliminate the cause of its occurrence.
The opinion of doctors. .. "
Absolute prohibition concerns the use of alcohol, restricting fats in the diet to 50 g, i.e. up to 15% of the total energy value of food consumed during the day. To make up for omega-3 fats, you should use linseed oil for pancreatitis. The menu should be simple and have a high energy value, about 2500 kcal. The portability of raw vegetables and fruits is individual, so you can give the patient boiled vegetables and baked fruit, for example, apples. It is important that the food contains a sufficient amount of fat-soluble vitamins and B vitamins. It is recommended to introduce antioxidant vitamins such as C and E.
Changes occurring in the pancreas as a result of chronic inflammation are irreversible. The goal of dietary treatment is to prevent the emergence of a deficiency of nutrients, vitamins and minerals.
5 Useful products of
There are a number of products that allow a diet for pancreatitis and cholecystitis:
- milk and milk products: milk, non-fat curd, yogurt, kefir, buttermilk;
- meat and fish: lean meat, for example, turkey, chicken, veal, beef;lean fish( cod, pollock);
- eggs: boiled soft-boiled, scrambled eggs or fried eggs;
- grain products: white bread, pasta and cereals, white rice, biscuits;
- vegetables: boiled carrots, pumpkin, beets, potatoes, young beans, green peas and cauliflower, raw carrots and tomatoes without skins);
- fruits: bananas, apples, peaches, apricots, oranges, raspberries, strawberries and currants in the form of mousse or puree;
- fats: linseed, rapeseed, olive oil;
- spices: salt, sugar, dill, marjoram, cumin, thyme, cinnamon, basil, rosemary, vanilla or lemon juice;
- sweets: sugar, honey, compotes, jam or puree fruit pitted, jelly;
- drinks: weak tea and coffee, milk, fruit or vegetable juices, herbal infusions and teas.
6 What should I avoid?
Foods that can not be eaten with pancreatitis and cholecystitis:
- milk and dairy products: fatty cheeses, for example, yellow cheeses;
- meat and fish: fat meats, for example, lamb, pork, duck, fatty sausages;
- eggs: fried with the addition of fat;
- cereal products: rye bread, wholemeal bread and whole grains, croissants, confectionery, cereals and whole grain pasta;
- vegetables: onions, spring onions, peppers, radish, cucumbers, pickled vegetables, horseradish;potato in the form of chips, fried, all legumes;
- fruits: gooseberries, plums, pears, sweet cherries, dried fruits and nuts;
- fats: fat, sour cream, solid margarines;
- spices: all sharp;
- sweets: chocolate, halva and other sweets containing fat, sugar, cocoa or nuts;
- drinks: strong tea and coffee, all kinds of alcoholic drinks, carbonated drinks.
Each time, you should monitor the body's response to consumed foods. It happens that some products on the banned list are well tolerated by the patient, for example, some vegetables, fruits or cereals. Be careful!!!
- 1 Clinical picture
- 2 Proper nutrition
- 3 Chronic course of the disease
- 4 Recommendations
- 5 Useful products
- 6 What should I avoid?
The diet for pancreatitis and cholecystitis is an important part of the treatment of these diseases. Drug therapy will not bring good results if the patient does not comply with the therapeutic diet.



