What is it? Rheumatoid polyarthritis is a common form of arthritis, a steadily progressing pathology from a group of immunogenic inflammatory diseases of connective tissue with a pronounced destructive component, a predominant joint damage and involvement of internal organs. According to the International Classification of Diseases of the 10th revision( ICD 10), rheumatoid polyarthritis is classified as inflammatory arthropathy.
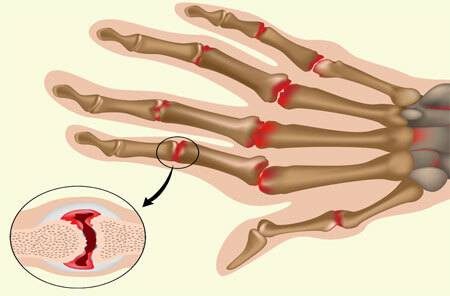
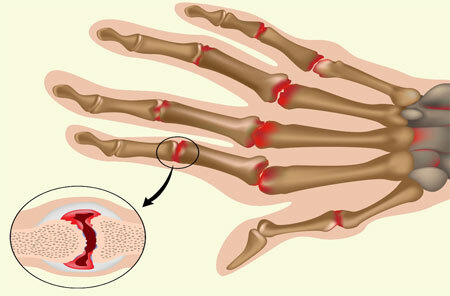
It affects small( metacarpophalangeal, interphalangeal and metatarsophalangeal) joints, but it can also affect large ones. It is accompanied by a violation of motor functions and leads to a loss of ability to work.
Contents
- 1 Causes of rheumatoid polyarthritis
- 2 Signs and symptoms of rheumatoid polyarthritis
- 3 Diagnosis
- 4 Treatment of rheumatoid polyarthritis
- 5 Complications of rheumatoid polyarthritis
Causes of rheumatoid polyarthritis
Rheumatoid polyarthritis is a disease that usually occurs over the age of 20 years. Most often it is diagnosed in women. The etiology is not fully established. The main reason is the failure of the functioning of the immune system, the cells of which begin to perceive the articular cartilages and the structures adjacent to them, as an alien object.
As a result, the protective mechanisms of the body are activated, the immune cells attack the connective tissue, slowly destroying it, causing severe deformations of the musculoskeletal system. Immunogenetic theory is considered the most probable.
There are many factors that trigger the development of the disease:
- hypothermia;
- metabolic disorders in the body;
- latent sluggish infection;
- joint injury;
- exposure to toxic substances;
- hormonal changes in the body;
- constant stress.
More often rheumatoid polyarthritis occurs in people with a genetic predisposition. The starting role in the development of pathology can play: chronic foci of infection, food allergy, physical overload.
Signs and symptoms of rheumatoid polyarthritis

Growing stiffness in the morning, swelling of the joints and minor pain in them during movement - the initial symptoms of rheumatoid polyarthritis. At first glance, they are quite harmless, but it all ends with deforming the joints. Mostly small hand and foot joints are involved, the process is symmetrical.
The disease is characterized by a chronic progressive course with almost no light periods. There is a tendency to relapse. In the synovial membrane, granulation tissue is formed and expanded, which destroys the cartilage and other parts of the bones with the appearance of erosion.
In addition to the joints, the muscle tendons are also involved in the process. On the back of the hands, with the course of the disease, the muscle mass atrophies, subluxations occur in the joints, resulting in the fingers deflecting to the outside, forming the form of a "walrus fin" or "rheumatoid brush."
The same happens with the foot. The defeat of small joints leads to the development of flat feet, hammer-shaped deformation of the fingers and their deflection outward. This is how the "rheumatoid stop" is formed.
As a result of the development of sclerotic changes, bone ankylosis appears. That is, the joint is deformed and becomes stiff. Among the possible nonspecific symptoms are: sweating, lowering blood pressure, general weakness, weight loss, lack of appetite.
Also to the symptoms of rheumatoid polyarthritis are:
- Constant pain intensification at night, with weather change;
- Formation of dense nodules in soft tissues near the affected joint;
- Trophic skin changes over a sore spot( redness, hair loss, nail change);
- Defeat of small vessels( rheumatoid vasculitis);
- Osteoporosis of bones;
- Local temperature increase;
- Pain in the cervical spine.
Many patients have a rheumatoid factor in their blood. This form of the disease is called rheumatoid seropositive polyarthritis. Its course is more severe and less favorable in the prognostic plan.
The destructive changes and violations of the joints functions are more pronounced, contractures and ankylosis are more often observed in comparison with seronegative polyarthritis.
Diagnosis

At the present stage, the diagnosis of rheumatoid polyarthritis is based on clinical, laboratory and instrumental methods. A rheumatologist after a history and examination can appoint a number of studies:
- X-ray examination - the gold standard for diagnosing erosion;
- Magnetic Resonance Imaging( MRI);
- ultrasound examination;
- general blood test;
- test for antibodies to cyclic citrullinated peptide;
- blood test for the presence of rheumatoid factor.
Since the disease attacks small joints, it is recommended to undergo an x-ray of hands and feet. In many cases, the method makes it possible to detect joint damage when only bone elements are drawn into the pathological process.
Approximately two years after the first symptoms, erosive changes become noticeable on X-rays. Traditional radiography can not fully meet the needs of medicine in assessing changes in the tendon-ligament apparatus and soft tissues.
In this respect, the most reliable method is MRI, which allows to identify inflammatory changes in the early stages of the disease. The method is used to examine patients with suspected rheumatoid polyarthritis as an alternative to radiography.
Evaluate soft joint tissues, cartilaginous tissue, ligaments, tendons and neurovascular bundles also allows ultrasound. The study is easily accessible, fast and economical. It makes it possible to visualize the minimum amount of effusion in the joint cavity, to detail the degree of change in the synovial membrane, and to conduct dynamic observations during the treatment.
In rheumatoid arthritis, the active inflammatory process can be confirmed by a general and biochemical blood test. The disease is characterized by an increase in the number of platelets, a low amount of albumin in the blood, a high rate of erythrocyte sedimentation.
As a sign of the disease, a positive rheumatoid factor may be considered, but its presence in the blood can not be the only diagnostic criterion.
An antibody test for citrulline-containing peptides is considered highly effective for the diagnosis of polyarthritis. The appearance in the bloodstream of antibodies is ahead of the appearance of signs of pathology for many years and allows you to forecast its course. The study is prescribed by a therapist, traumatologist, orthopedist.
Treatment of rheumatoid polyarthritis

In rheumatoid polyarthritis, the treatment is based on the combined use of methods of physiotherapy, reflexology and homeopathy. Therapy is aimed at:
- Elimination of the inflammatory process;
- Reducing pain;
- Restoration of functioning of the affected organs;
- Correction of immunity disorders;
- Increased life expectancy;
- Achieving remission of the disease.
At the first stage of treatment, the main task is to rationalize the menu. In rheumatoid polyarthritis nutrition and diet should be restorative, depending on the phase of the disease, the degree of involvement of internal organs and the presence of complications.
Observing the diet can reduce inflammation and correct metabolic disorders. During the period of exacerbation, it is advisable to reduce the amount of easily digestible carbohydrates( honey, sugar, jam), to limit the intake of proteins, animal fats and salt.
You can not eat foods that excrete calcium: sorrel, rhubarb, spinach. Food should be cooked in boiled or baked form.
Dietary food completely excludes alcoholic beverages, meat and fish broths, pickles, marinades, spices and condiments.
Treatment with medications is prescribed individually. The basis of therapy is drug-induced immunosuppression. Immunosuppressive drugs for the treatment of rheumatoid polyarthritis include:
- Basic anti-inflammatory drugs( methotrexate, leflunomide, sulfasalazine, hydroxychloroquine, cyclosporine);
- Biological preparations( infliximab, rituximab, abatasept);
- Glucocorticosteroids( prednisolone, dexamethasone).
On the second level of , non-steroidal anti-inflammatory drugs are effective: nimesulide, diclofenac, meloxicam, ibuprofen. For local symptomatic therapy, preparations are used in the form of ointments and gels.
Patients with an established diagnosis of rheumatoid polyarthritis should be prescribed a drug from the group of basic anti-inflammatory drugs, other medications are used as needed. Treatment is carried out only under the supervision of a rheumatologist, long-term therapy, which implies periodic monitoring of the activity of the disease course and evaluation of the response to therapy.
Physiotherapeutic methods use electrosleep, UF in erythematous doses around the affected joint, mud treatment, hydrogen sulphide baths, massage, magnetotherapy, physiotherapy exercises.
Objectives of physiotherapy rehabilitation:
- Prophylaxis of subsequent disruption of joint function;
- Improving the performance of the muscular system;
- Reducing pain;
- increased metabolism;
- Fighting muscular atrophy;
- Improvement of blood circulation in the joints.
Physiotherapy methods are used at various stages of the disease. In most cases, they make it possible to achieve concrete success in treating the symptoms of rheumatoid polyarthritis and do not cause negative side effects.
The immune system can be resumed using computer reflexotherapy. The essence of the method consists in the action of an ultra-low direct current on biologically active points, which have a connection with the brain through the autonomic nervous system.
Reflexotherapy promotes more rapid elimination of spastic conditions, elimination of pain and inflammation.
In case of treatment-resistant polyarthritis and severe deformities, surgical intervention is indicated.
Complications of rheumatoid polyarthritis
Rheumatoid polyarthritis may accompany secondary complications - extra-articular manifestations, which sometimes come to the fore in the overall picture of the disease.
This includes:
- serosites( inflammation in the pleura and pericardium);
- diffuse glomerulonephritis;
- lymphadenopathy;
- pyelonephritis;
- chronic pneumonia;
- peripheral neuropathy;
- kidney damage in the form of amyloidosis;
- dry Sjogren's syndrome;
- myocardial dystrophy.
In rheumatoid arthritis, disability very quickly occurs, and various infectious complications with severe course and renal insufficiency often lead to a lethal end.
To avoid complications, it is important not to miss the time when you can still stop the deformity of the joints and not delay treatment.