The largest anatomical education from the connective tissue begins at the confluence of the heads of the triceps gastrocnemius muscle. It is located at the calcaneus and is called the Achilles tendon.
Record content:
- 1 Achilles tendon anatomy, structure, location
- 2 Functions of the Achilles tendon
- 3 Diagnosis of tendon pathologies
-
4 The main diseases of the Achilles tendon, their symptoms and treatment
- 4.1 Tendinitis
- 4.2 Paratendinitis
- 4.3 Bursitis
-
5 Achilles tendon injuries, their signs, conservative and surgical treatment
- 5.1 Tear
- 5.2 The gap
- 6 Rehabilitation after treatment of diseases and injuries
- 7 Achilles Tendon Disease Video
Achilles tendon anatomy, structure, location
Achilles or calcaneus tendon is formed from the aponeuroses of the calf and soleus muscles. The plantar tendon extends to the medial surface just proximal to the seam and extends distally to the insertion site.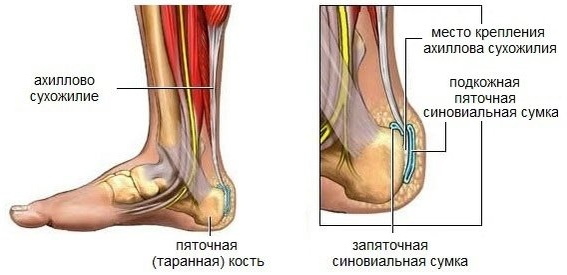
The Achilles tendon has no synovium. Instead, it is surrounded by vascularized paratenon, a transparent membrane consisting of a single layer of cells and a membrane of loose areolar (connective) tissue rich in mucopolysaccharides.
Paratenon is adjacent to the muscle fascia and merges with the periosteum of the calcaneus. The structure of the sheath allows the tendon to slide relative to adjacent anatomical structures, retreating 1.5 cm.
The blood supply in this area is formed by the network of arteries within the paratenon. Most of the tendon is supplied with branches of the posterior tibial artery. Its middle part is supplied with branches from the peroneal artery.
The Achilles tendon is located in a place that takes a huge load when a person moves. But at the same time, this same area is the most vulnerable and traumatized.
Functions of the Achilles tendon
The calf and soleus muscles, which act through the heel tendon, are the main flexors of the ankle joint.
They provide the primary driving force during:
- running;
- walking;
- jumping.
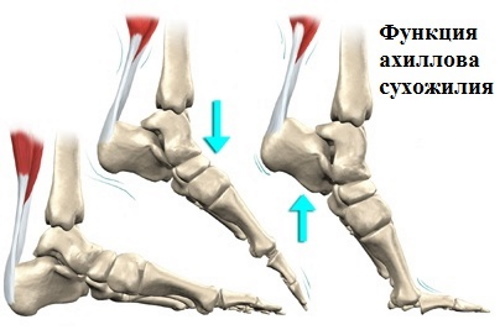 In addition, the soleus muscle helps prevent roll or fall forward when standing. Contraction of the triceps femoris also promotes knee flexion and supination of the subtalar joint. The main task of the Achilles tendon is to transfer force to the foot and heel from the triceps muscle.
In addition, the soleus muscle helps prevent roll or fall forward when standing. Contraction of the triceps femoris also promotes knee flexion and supination of the subtalar joint. The main task of the Achilles tendon is to transfer force to the foot and heel from the triceps muscle.
While walking, the Achilles tendon experiences dynamic loads that are 2-3 times the body weight, and when running, its strength increases 12.5 times.
Diagnosis of tendon pathologies
When diagnosing a disorder in the area of the calcaneal structure, the doctor asks questions about the nature of the pain and conducts a physical examination:
- Palpation involves examining and pressing around the painful area for swelling, warmth, crepitus (cotton sensation), which is characteristic of acute tendinitis.
- As part of the physical examination, a Thompson test is performed to determine a complete rupture. It is performed by squeezing the calf.
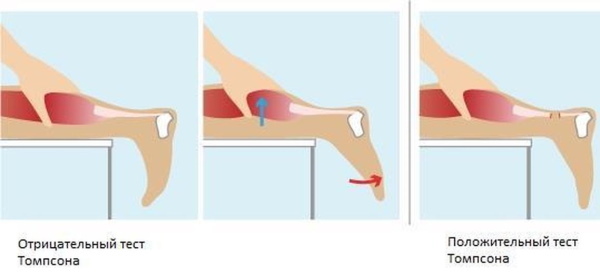
- The Matles test is a visual screening that is done when a tendon rupture is suspected.
- MRI and ultrasound are also prescribed if there is a suspicion of detachment of the attachment point to the calcaneal tubercle.
The main diseases of the Achilles tendon, their symptoms and treatment
The Achilles tendon is located in an area that is prone to frequent injury during overload, especially in athletes and older people. The most common types of injuries, accounting for 55–65% of cases, are associated with tendinopathy.
The development of bursitis in the calcaneal region accounts for 25–35%, in other cases, partial and complete ruptures are diagnosed.
If a tendon is damaged, conservative treatment is most effective. This includes maintaining a state of rest, applying cold, compressing and raising the leg, which are done immediately after the injury.
| Pain relief method | Action |
| Rest | Do not press on the damaged area for 1-2 days after the injury, until the pain goes away. |
| Cold | Ice should be applied to the injury site, placed in a bag wrapped in cotton cloth. They keep the cold on the tendon for 15–20 minutes, then it is removed so that the injury site heats up again. Ice accelerates the relief of inflammation or swelling. |
| Compression | A bandage or elastic band wrapped around the tendon prevents excessive swelling of the limb. To avoid restricting blood flow, the dressing should not be too tight. |
| Climb | A foot located above the level of the heart will help blood circulate normally and thus reduce swelling. |
With minor injuries, treatment does not take more than 2-3 days, and full recovery occurs in 5-6 weeks.
Achilles tendon injuries are also common in non-athletic people and often result from a combination of factors including:
- excessive stress;
- changes in biomechanics;
- degeneration of tendons.
These pathways of injury affect the heel and the surrounding structure in different ways.
Tendinitis
Permanent microtrauma that occurs between the gastrocnemius and soleus muscles cause an abnormal concentration of load in the tendon, which leads to inflammation and degeneration of the tendon sheath. Without appropriate treatment, spending the necessary time for recovery, tendinopathy may develop.
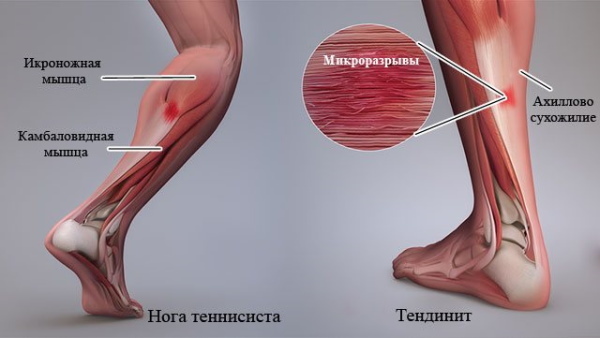
Damage symptoms:
- Pain, often described as a burning sensation that gets worse with physical activity. The location of the pain can be different. Sometimes it is felt closer to the lower part of the calf muscle, in some cases along the tendon itself or below, near the calcaneus.
- There is slight swelling and warmth in the affected area.
- Morning stiffness appears, both in the heel and in the calf. Relief comes when the person warms up or does ankle and leg stretch exercises.
- Other symptoms include constriction of the calf muscles and limited range of motion when flexing the foot.
To reduce pain, NSAIDs are prescribed, medications have proven themselves well:
- Nurofen Plus. The anti-inflammatory drug is recommended to take 1 tab. 3-4 times / day.
- Ibuprofen. The non-steroidal drug is used in this case at 1600-2400 mg 1 time / day.
Corticosteroid injections are not recommended in such cases.
After the inflammation and pain has been relieved, it is recommended to start calf strengthening exercises such as calf raises, toe balancing, and wall stretching. Eccentric strength training (toe push-ups and slow lowering) is a popular and beneficial treatment option, as is deep calf and soleus massage.
In case of ineffectiveness of conservative therapy, an operation may be required:
- Open plastic. During the operation, the surgeon makes an incision above the heel bone. Then the 2 sides of the torn tendon are sutured and the incision is closed.
- With the closed method, the surgeon does not make a longitudinal incision in the skin. In this case, laparoscopic equipment is used.
- Recovery from surgery can take anywhere from a few weeks to several months.
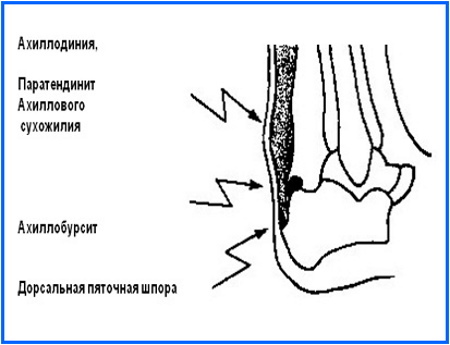
Paratendinitis
The Achilles tendon, which constantly receives microtrauma, undergoes inflammation of the membrane that is located around the connective tissue, which contributes to the development of paratendinitis.
The main symptoms are:
- pain and stiffness;
- limited range of motion of the leg;
- swelling, fever at the site of inflammation;
- crackling sound when moving or palpating the affected area.
Paratendinitis limits the ability to walk, stand for long periods, or climb stairs because of severe heel pain.
The first step in treatment is rest and rest for the affected leg for at least a week. Adaptive devices such as crutches are used to reduce weight on the tendon. Pain relievers are used to relieve pain, and some patients benefit from cold or hot compresses.
Once the initial pain and inflammation have subsided, physical therapy sessions are scheduled. The focus is on stretching and strengthening the muscles around the affected area to stabilize and support the tendon and prevent re-injury.
If the above procedures do not reduce inflammation, your doctor may prescribe corticosteroid injections to reduce pain and inflammation in the affected joint.
Bursitis
The Achilles tendon is where fluid-filled bursae are present. Bursitis, or bursitis, is common in athletes. Also called retrocalcaneal bursitis, the disease affects a small sac that sits between the Achilles tendon and the heel bone, known as a bursa.
The heel bag contains a lubricating fluid, acts as a cushion, and reduces friction between muscles and bones.
In the heel area there are 2 separate sacs, the disease proceeds depending on which one is inflamed:
- Anterior bursitis. In this case, the thin pad located between the calcaneus and the calcaneal tendon is affected. Over time, inflammation can spread to the entire heel.
- Posterior bursitis, which affects the outer pad located between the heel tendon and the skin. If left untreated, the outer bursa can become hard and scar-like.
Posterior bursitis symptoms:
- pain, swelling, and warmth in the back of the heel;
- worn out top layer of leather on the heel;
- the formation of a flesh-colored nodule in the affected area;
- the development of scar tissue.
Anterior bursitis symptoms:
- pain, warmth in the back of the heel;
- Difficulty walking in shoes
- a small red spot on the back of the heel, tender to the touch;
- swelling that spreads to other parts of the heel

Treatment methods:
| Medicinal | High-dose NSAIDs. |
| Injections of corticosteroids + anesthetics into the area of the inflamed bursa (from 0.5 to 1 ml, for example, triamcinolone acetonide 40 mg / ml) + 2% lidocaine solution. | |
| Home | Warm or cold compresses Wearing comfortable shoes, special insoles, inlays (for posterior tendon bursitis). |
| Aspiration of liquid | In this case, a syringe is inserted into the joint and the excess fluid accumulated in the swollen bag is sucked off. It helps relieve pain, swelling, and relieve pressure. After removing the fluid, glucocorticoids are administered. |
| Microcurrent therapy | Therapies with the CellVAS device |
| Physiotherapy | Restores and improves flexibility and strength of muscles, tendons and joints around the ankle. |
| Surgery | Bursectomy is a surgical procedure performed to remove an inflamed or infected bursa. |
 Other surgical procedures may be required depending on the cause of the calcaneal bursitis and associated symptoms. This can include correcting the deformity of the foot, removing bone spurs, correcting any other changes in the bone or soft tissues that caused heel bursitis.
Other surgical procedures may be required depending on the cause of the calcaneal bursitis and associated symptoms. This can include correcting the deformity of the foot, removing bone spurs, correcting any other changes in the bone or soft tissues that caused heel bursitis.
Achilles tendon injuries, their signs, conservative and surgical treatment
Achilles tendon ruptures are classified into 4 types, depending on the severity and severity of the rupture:
- Type I: Partial tears ≤50% - usually treated conservatively.
- Type II: complete with tendon rupture ≤3 cm - treated with end anastomosis.
- Type III: complete with a tendon rupture of 3 to 6 cm - often a tendon (synthetic) graft is required.
- Type IV: complete rupture with a defect> 6 cm (advanced forms) - Tendon recession (synthetic graft) of the gastrocnemius muscle is required.
Tear
Partial separation can occur in athletes of all sports, dancers, and the elderly. In this case, the injury occurs at the site of attachment of the tendon to the calcaneal tuberosity.
Partial rupture symptoms:
- Sudden, sharp pain in the back of the leg.
- Pain that disappears when the muscles are warmed up during exercise, but returns after exercise.
- Rigid tendons in the morning.
- Edema.
Treatment:
- Apply cold, compression, leg lift and rest for the first 3 days.
- Using crutches when walking.
- Local administration of 0.5-1% novocaine solution.
- Plaster cast. In this case, the plantar flexion of the foot and knee joint should be at an angle of 145˚.
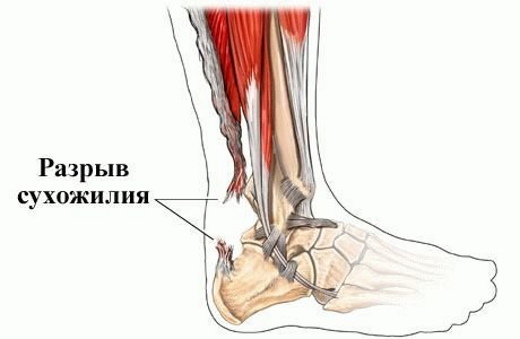
The gap
The Achilles tendon is located behind the ankle and is a strong fibrous cord, complete ruptures of which are more common in athletes.
With a complete rupture, one feels:
- pop or pop;
- sharp pain in the back, just above the heel;
- increase in edema,
- stiffness and difficulty standing up on tiptoe and pushing the leg while walking;

Treatment depends on the severity of the injury, the person's age, and their level of activity. Young people, especially athletes, are more likely to undergo surgery to recover completely torn fibers, whereas older people are more likely to choose nonsurgical treatment, immobilization in plaster.
- Non-surgical treatment involves wearing a cast or a special brace that lifts the heel and allows the tendon to heal.
- The surgical procedure involves opening the skin and suturing the torn tendon. Surgery reduces the number of Achilles tendon recurrences compared to non-surgical treatments.
 With any subsequent treatment, physical therapy is recommended to increase the strength and flexibility of the leg muscles. However, a non-surgical approach increases the chance of re-rupture, and recovery may take longer.
With any subsequent treatment, physical therapy is recommended to increase the strength and flexibility of the leg muscles. However, a non-surgical approach increases the chance of re-rupture, and recovery may take longer.
After the plaster is removed, physiotherapy sessions are performed, which begins with mild passive mobilization of the ankle and subtalar joints.
After 2 weeks, progressive resistance exercises are added:
- Active flexion - extension of the ankle.
- Circles around the ankle (clockwise and counterclockwise).
- Hip abduction.
- Raising a straight leg.
- Standing hamstring flexion.
- Riding a stationary bike.
Rehabilitation after treatment of diseases and injuries
Bringing the tendon into working condition is one of the methods of treatment. For tendinopathy, physical therapy can relieve pain. If a rupture occurs, a postoperative recovery program may be required. More often, after injury, a plaster cast is applied to heal the tendon. After the cast has been removed, usually after 6-8 weeks, rehabilitation can begin.
Physiotherapy and various sets of exercises are prescribed to help healing:
- Stretching and flexibility exercises are necessary to increase the range of motion, reducing the risk of new injury.
- Strengthening exercises can help restore strength lost during joint healing.
Endurance exercises such as stationary bike riding can be added to the rehabilitation program. Other physical therapy treatments include ultrasonic heat therapy to improve circulation and healing, and deep massage to increase leg flexibility.
Postoperative rehabilitation involves avoiding abrupt, active movements for 10-12 weeks. You should closely monitor the mobility of the tendon, the condition of the seams and signs of scar tissue formation. At 4 weeks, scar mobilization can begin as soon as the incisions are completely closed. Running, jumping and ballistic exercises are prohibited for 6 months.
Over the first 3-8 weeks, you should gradually increase the weight bearing as appropriate and depending on the range of motion. After 6 weeks, an increase in passive range of motion and extension of the Achilles joint are gradually added. At week 6, you can add an exercise bike with just a heel.
At 10-12 weeks, the physical therapist suggests starting isometric exercises to achieve full movement of the ankle.
Exercises are carried out from 3 to 6 months:
- controlled squats;
- lunges;
- bilateral calf lifting (transition to unilateral);
- rise on toes.
Starting at 6 months old, you can jog, jump and do eccentric loading exercises. At 8-9 months, patients usually return to work or strenuous sports.
Restorative procedures are approximate, based on the individual characteristics of the patient, which are evaluated throughout the entire treatment process.
Achilles tendon problems can vary in both developmental and treatment. One of the important tasks is to determine whether the cause of the disorder is trauma, inflammation, or the pathology is in the stage of chronic degeneration. The correctness and effectiveness of the prescribed treatment depends on this.
Achilles Tendon Disease Video
Achilles tendon inflammation:



