 Epilepsy in various forms affects approximately 1% of the population, and various sleep disorders - up to 50%, which, in itself, involves relatively frequent coincidence and interaction.
Epilepsy in various forms affects approximately 1% of the population, and various sleep disorders - up to 50%, which, in itself, involves relatively frequent coincidence and interaction.
The mutual influence of epilepsy and sleep is much deeper, more complex and more frequent than just an accidental coincidence. The relationship between sleep and epilepsy is of clinical interest to scientists since antiquity.
Content
- Historical background
- Night seizures
- forms of attacks specific to sleep
- Autosomal dominant nocturnal frontal epilepsy
- Epilepsy with centrotemporal spikes
- Electric epilepticus of sleep status
- syndrome of acquired aphasia, Landau-Kleffner
- Idiopathic generalized syndromes
- Impact of attacks on sleep
Historical excursion of
Aristotle in the 4th century BC.expressed the opinion that "sleep is like an epileptic seizure."Today it is known that epileptic seizures are clinical manifestations of hypersynchronous central neuronal activity, and the coming sleep is also characterized by changes in the synchronicity of the action potential of CNS neurons.
Galen in the 2nd century BC.stressed the importance of sleep for patients with epilepsy, and warned of the inexpediency of daytime nap. 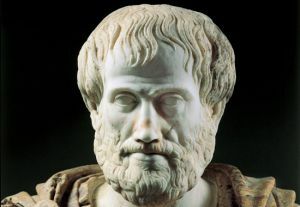 Today it is known that the REM-phase of sleep and awakening can act as a stimulus for an attack.
Today it is known that the REM-phase of sleep and awakening can act as a stimulus for an attack.
Gauers examined a group of epileptic patients at the beginning of the 20th century and found that 42% of cases were characterized by exceptional daytime seizures, 21% - exclusively by night and 37% by seizures, regardless of the time of day.
Today it is known that some epileptic syndromes and seizures have a close connection with the sleep and wake cycle.
Epileptic seizures disturb sleep and, conversely, sleep disturbances( eg, sleep apnea) can trigger an attack. In addition, the effect of antiepileptic drugs on sleep is essential.
Epilepsy, some of which have the nature of nosological units and syndromes, manifests itself in various types of epileptic seizures. There are, like "normal" epileptic seizures, and epilepsy, directly related to sleep.
Nocturnal epileptic seizures
People often describe various events related to sleep. The first decision the physician needs to analyze the  for a specific nighttime condition is to determine if there is a physiological phenomenon of sleep or a pathological manifestation.
for a specific nighttime condition is to determine if there is a physiological phenomenon of sleep or a pathological manifestation.
If the description of the condition is outside the normal manifestations of sleep, the next step is to differentiate epileptic seizures from sleep disorders( parasomnias, difficulty breathing during sleep, periodic movement of the legs during sleep), psychogenic attacks, secondary manifestations of internal diseases and other diseases.
Epileptic seizures in a dream have 3 features:
- they are rarely observed, and it is more difficult to obtain an accurate description of the seizure seizures;
- nocturnal seizures disturb sleep, which in turn affects daytime functionality and activity;
- nocturnal seizures are easily confused with parasomnia, other somnological seizures, or take them for a mental disorder.
A symptom that determines the nature of nocturnal epileptic seizures is the stereotyped, recurring nature of seizures, the simultaneous occurrence of daily and nighttime seizures and the determination of specific epileptic activity in the EEG.
sleep patterns There are several forms of sleep related attacks:
- Frontal , which is characterized by a dystonic manifestation on the limbs, possibly a voice manifestation, rotational movements or complex motor activity( hypermotoric attacks).
- Temporal often occur in a complex combination of complex motor manifestations - automatic, autonomic and psychological symptoms.
- Nuchal is characterized by visual symptoms, eye movements, sometimes vomiting and headaches.
Nocturnal manifestations of epilepsy in sleep dominate in relation to frontal seizures. Also known are several epileptic syndromes and disorders closely related to sleep.
Autosomal dominant night frontal epilepsy
The pathophysiological basis of this disease is the gene defect for the 4th subunit of the acetylcholine receptor on chromosome 20, which causes recurrent night attacks with hyperkinetic symptoms and dystonia, frequent awakenings, and in 2/3 patients with tonic-clonic convulsions.
Seizures begin, mostly at the age of 7-12 years, and occur several times a night( mostly after falling asleep or before awakening).As a rule, they are a family phenomenon.
Epilepsy with centro-temporal adhesions
The most common childhood epilepsy affecting 10-20 / 100000 children, also called benign Rolandic  epilepsy, occurs in children 5-12 years old with hemifacial tonic convulsions and paresthesia, swallowing, salivation and speech stopping.
epilepsy, occurs in children 5-12 years old with hemifacial tonic convulsions and paresthesia, swallowing, salivation and speech stopping.
Consciousness, as a rule, is present. Rolandic seizures can progress to tonic-clonic convulsions.
Benign epilepsy with centro-temporal adhesions is typical, associated with age, syndrome. Attacks occur in the non-REM sleep phase, usually after falling asleep or before awakening, and spontaneously disappear with the onset of puberty.
Electrical sleep epileptic status
This definition represents another disease related to childhood, encephalopathy, characterized by continuous epileptic activity in delta sleep, seizures and delayed psychomotor development.
The disease begins at the age of 2 months to 12 years. The components of the disease are polymorphic seizures, including hemifacial convulsions, hemiconvulsions, myoclonic and atonic attacks, mainly occurring at night.
During the course of the disease, a progressive disturbance of neuropsychological functions( hyperkinetic symptoms, agitation, aggressiveness, attention deficit disorder, deepening of mental retardation with speech disorders) is manifested.
Syndrome of Acquired Aphasia of Landau-Kleffner
The basis of this disease is auditory verbal agnosia caused by epileptic activity affecting the sensory speech center of the dominant temporal field of Wernicke in a sensitive period of ontogenetic development from 2 to 8 years.
The disease activates the focal epileptic activity of the posterior temporal region, which, again, manifests itself in the non-REM sleep phase.
Idiopathic generalized syndromes
Epilepsy with GM bouts on waking and juvenile myoclonic epilepsy Two syndromes partially overlapping refer to idiopathic generalized epilepsy( genetically determined, with normal results of MRI of the brain).
Epilepsy on waking is clinically manifested, mainly on the 2nd 10th anniversary of life. Generalized tonic-clonic seizures are exclusively or predominantly activated shortly after awakening( within 1 hour, regardless of time of day).
Parallel with this, other types of seizures( myoclonus) may appear. The provoking factor is often deprivation of sleep. 
The main symptoms of UME are myoclonic twitching( shoulders, upper extremities), generalized tonic-clonic seizures( & gt; 90% of patients), and, in some cases, unconsciousness( about 30%).
Clinical manifestations begin, mainly, at the age of 12-18 years. JME often manifests itself in the first half of the day, within 1 hour after awakening.
The most important factor triggering seizures is sleep deprivation( especially when it is associated with a forced early rise from bed) and alcohol consumption.
The effect of seizures on
sleep. Night attacks disrupt the sleep and wake cycle, which leads to postictal drowsiness. Fragmentation of sleep is more severe in focal epilepsy.
The effect of antiepileptic drugs on the structure of sleep is controversial. In the first generation of PEP( barbiturates), a nonspecific oppressive effect predominates. Carbamazepine and other PEPs acting as a sodium channel blocker improve  sleep fragmentation.
sleep fragmentation.
Valproate improves the N3 deep sleep phase and reduces the REM phase. Lamotrigine may cause subjective feelings of insomnia, but during polysomnographic studies, objective deterioration of sleep has not been confirmed.
With respect to Topiramate, subjective fatigue was observed. Pregabalin changes the structure of sleep - increases the proportion of REM due to N2( non-REM2).
Sleep and epilepsy have very complex relationships. Sleep is an essential human need, like air, water and food.
Most patients with epilepsy have a combination of daytime and nighttime seizures, and cases with a predominance of nocturnal seizures are rare. Thus, the issue of nightly calm in patients with epilepsy and their home observation is very important.