 Intracranial hypertension is a life-threatening condition of its early detection and treatment are essential for the survival of patients.
Intracranial hypertension is a life-threatening condition of its early detection and treatment are essential for the survival of patients.
Intracranial hypertension( VH) is defined as an increase in intracranial pressure( ICP) above physiological levels with normocapnia. The
ICP for the adult population is up to 15 mmHg. The prognosis of patients with VH is based not only on survival, but also on long-term permanent neurologic complications.
The treatment strategy is based on early diagnosis, identification and treatment of the causes, therapy / elimination of secondary intracranial and extracranial ischemic strokes and surgical interventions, in the case of their indications.
Contents
- Pathophysiology of a disorder
- Causes and risk factors for a violation
- Elevated ICP in children - what, how and why?
- Clinical picture and main symptoms
- Indirect signs of intracranial hypertension
- Qualitative diagnostics
- Methods of therapy
- Benign intracranial hypertension
- Danger in itself is. ..
Pathophysiology of violation
The volume of the intracranial space of an adult person is about 1500 ml and consists of brain tissue( 80%),cerebrospinal fluid( 10%) and blood component( 10%).
With depletion of compensatory mechanisms, even with a small increase in volume, the rapid increase in ICP occurs with a decrease in perfusion brain pressure( PMD).PMD is determined by the difference between systemic mean arterial( SBP) and intracranial pressure( PMD = SBP - ICP).
The optimal value of PMD to maintain adequate perfusion of brain tissue is 60-70 mmHg under PMD.
Damage to the brain can be divided into primary and secondary. The causes of primary damage include brain contusions with concussions, hemorrhages, diffuse axonal lesions, cerebral strokes( ischemic or hemorrhagic), neuroinfections, tumors.
The main mechanism is the pro-inflammatory( pro-inflammatory) reaction with excessive activation of the secretion of the neurotransmitters 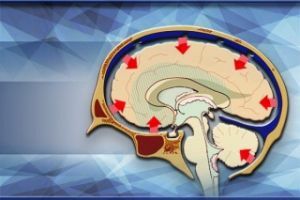 ( especially glutamate), pro-inflammatory cytokines and oxygen radicals.
( especially glutamate), pro-inflammatory cytokines and oxygen radicals.
It comes to uncontrolled influx of calcium, sodium and water intracellularly, activation of intracellular proteases, simultaneously increases the permeability of the blood-brain barrier, loss of autoregulation and progression of cerebral edema.
The result of these changes is mitochondrial dysfunction with depletion of adenosine triphosphatase and energy deficiency of cells. To the progression of brain damage are extracranial lesions: hypotension, hypoxemia, hyperglycemia / hypoglycemia, hypercapnia.
Causes and risk factors for
disorders The following causes are caused by the syndrome of intracranial hypertension:
- increase in the volume of brain tissue : what can be caused by expansive processes( tumors, inflammations, hematomas);as well as edema of the brain;
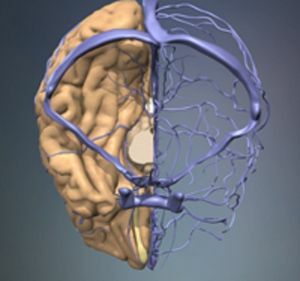
- increase in intravascular volume of blood : arterial loss of autoregulation, vasodilation induced by changes in pH and PaCO2 and worsening of venous outflow from the brain( sinus thrombosis);
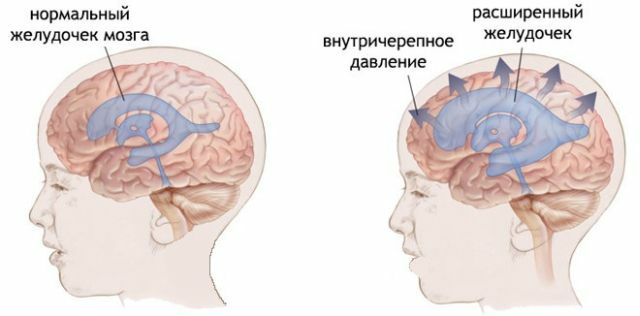
- increase in the volume of cerebrospinal fluid - hydrocephalus.
Diffuse edema of the brain differs, local and perifocal( around the tumor or ischemic focus of concussion).
For the pathophysiological aspects, the following forms of cerebral edema differ:
- vasogenic is a violation of the function of the blood-brain barrier, which becomes permeable to ions and water, with
 followed by fluid transguration. Capillary hydrostatic, oncotic and interstitial pressures are the main factors determining the degree of fluid transport;
followed by fluid transguration. Capillary hydrostatic, oncotic and interstitial pressures are the main factors determining the degree of fluid transport; - cytotoxic is the result of toxic or ischemic damage to brain cells;
- hydrostatic is a consequence of high blood pressure in the absence of a violation of the blood-brain barrier( hypertension, decompression after the evacuation of the intracerebral hematoma);
- osmotic is the result of an osmotic gradient in hypoosmotic serum;
- interstitial - present in patients with obstructive hydrocephalus.
Increased ICP in children - what, how and why?
Intracranial hypertension in infants manifests a convex fontanel, and with decompensated chronic hydrocephalus there is a divergence of the seam of the skull with a characteristic sound when tapping on it, which can be aligned with the sound when tapping a cracked pot( signe du pot félé), thus manifesting hydrocephalus of the skull.
With prolonged intracranial hypertension comes to a decrease in intelligence and, eventually, focal brain symptoms appear.
Reasons:
- primary brain tumors;
- metastasis of other tumors to the brain;
- infiltration of the spinal cord with tumor processes( leukemia, medulloblastoma), which leads to impaired absorption of cerebrospinal fluid( resorptive form of hydrocephalus);
- is not a cancer cause: infection( meningitis, abscess, subdural empyema), bleeding and trauma.
Clinical picture and main symptoms
 Clinical signs of intracranial hypertension include headache, nausea, vomiting, visual impairment, diplopia, quantitative and qualitative disorder of consciousness.
Clinical signs of intracranial hypertension include headache, nausea, vomiting, visual impairment, diplopia, quantitative and qualitative disorder of consciousness.
The symptomatology depends on the severity of the HH, the rate of development and the underlying cause. Some patients may have a so-called. Cushing's reflex characterized by arterial hypertension and wandering reflex bradycardia.
Indirect signs of intracranial hypertension
Children do not have cranial bones merged, and a slow increase in intracranial pressure can compensate for their tightening and enlarging the skull, this occurs without other symptoms.
In the case of a rapid increase in pressure, however, these mechanisms do not have time to exercise, and the pressure is reflected in the same way as in adults.
In adults, cranial bones have no escape routes, the skull is a rigid shell. The only large opening is in its lower part, through which the spinal cord exits.
With increasing intracranial pressure, a certain amount of cerebrospinal fluid recedes from the head, but there is no other reserve.
Therefore, excess pressure will begin to act on the brain. This is reflected in headache, dizziness, nausea and vomiting.
Various neurological disorders can be found - motor and sensitivity disorders.
Qualitative diagnosis
Diagnostics is based, in addition to clinical trials, mainly on visualization, the gold standard is the performance of CT of the brain;depending on the cause, further examinations can be performed - multimodal CT of the brain, MRI, angiography, etc.
Intracranial pressure is verified by measuring ICP by a sensor that is administered intravenously. With the progression of the HH reaches the hernia of the brain tissue with a stop flow through the vessels of the brain and brain death.
Therapy methods
The treatment of intracranial hypertension is based on the reduction of intracranial pressure, the elimination of secondary lesions and the treatment of  the underlying cause of the disease.
the underlying cause of the disease.
The basis for the complex treatment of intracranial hypertension is the reduction in the volume of individual areas: cerebrospinal fluid, blood, intercellular fluid, brain tissue.
The following procedures are used:
- External Ventricular Drainage .If VG is preserved, despite the above measures, the best choice is the method of drainage of cerebrospinal fluid, in particular, in the treatment of patients with obstructive hydrocephalus.
- Hyperventilation .Most often, with conservative therapy, manipulation with the volume of blood is used. Induction of mild hyperventilation with strict control of RaCO2( light hypocapnia 30-35 mmHg) causes the narrowing of blood vessels due to a decrease in the volume of blood in the brain. The risk of hyperventilation is to induce respiratory alkalosis and excessive narrowing of the blood vessels, which can lead to insufficient perfusion of the brain and deterioration of the condition.
- Osmotherapy .A rapid increase in osmotic serum leads to a displacement of fluid from the extravascular space to the vessels and reduces the volume of interstitial fluid in the brain. The mechanism of action is not entirely clear, as are side effects, which include the risk of acute renal failure.
- Decompressive craniotomy .In the absence of the effect of traditional therapy, in the treatment of intracranial hypertension, there is growing interest in the implementation of decompression craniotomy. Most often, the frontal-parietal-temporal-occipital surgery is performed, which is indicated for patients with craniocerebral trauma.
Treatment of early seizure activity( phenytoin, carbamazepine), correction of arterial hypertension( beta blockers), nutritional support, prevention and treatment of complications, prevention of stress ulcers, bleeding and deep vein thrombosis, correction of the internal environment and glucose are recommended for other supportive measures.
Benign intracranial hypertension
A benign HD is classified separately. This pathology is characterized by affecting young women( under the age of 25), mostly obese.
To date, the causes of the disease are unknown, sometimes they are associated with certain disorders:
- autoimmune diseases;
- endocrine disorders;
- leukemia;
- pregnancy;
- use of certain medications, especially corticosteroids and antibiotics;
- polycythemia;
- Lupus;
- iron deficiency anemia;
- chronic renal failure.
It is worth noting that a benign VG can disappear as suddenly as it does.
The danger in itself is thawing. ..
 The brain is the most important organ. When in a compressed state, it loses its ability to function normally. Can reach the atrophy of the brain substance, hence - to reduce the intellectual potential of man and nervous disorders of internal organs.
The brain is the most important organ. When in a compressed state, it loses its ability to function normally. Can reach the atrophy of the brain substance, hence - to reduce the intellectual potential of man and nervous disorders of internal organs.
If the pressure rises without taking the necessary measures, the brain under its influence squeezes into the hole in the base of the skull through which the spinal cord protrudes into the spinal canal. The brain begins to cling to the bony edges of the hole, which leads to its damage.
Unfortunately, the first in terms of damage is the oblong area, where vital centers are located, incl.respiratory center. The victim develops a violation of consciousness, which ends with stopping breathing and dying.
Timely treatment can stop the disease at an early stage, preventing its further development.
Preventive measures for the development of intracranial hypertension include the following:
- limit of consumed liquid to 1.5 liters per day;
- timely treatment of pulmonary diseases in order to ensure adequate airway patency;
- maintenance of acid-base, water and electrolyte balance;
- timely treatment of hypertension, hyperthermia, epilepsy;
- minimizing the use of drugs that have vasodilating properties.



